 02-24-2019, 07:30 PM
02-24-2019, 07:30 PM
EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA

 EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
PART 1
THE GOOD
I am recapping an earlier post I made to provide context for this post.
To begin, I would like to say that I love the Airfit P10 for its innovative solution to the problems with the headgear and vents of traditional nasal pillows.
I am a physician and have used well over 20 different products from full face to nasal mask and pillows since being diagnosed with OSA. I finally settled on the Resmed AirSense 10 Autoset and P10 pillows.
I found that its light weight, split head strap resulted in much improved lateral stability over the usual pillow design, which tended to pull upward and back. This was necessary because of the need to provide upward tension against the nostrils. The price was less lateral stability and leaks. This was compensated for with beefier straps for pulling the head gear tighter, resulting in discomfort and the inevitable depression marks on your face. The P10 headgear pulls both upward and downward resulting in force vector more directly backward from the nose while still maintaining a good seal. This creates a four-point restraint that makes the pillow much less prone to being dislodged by any lateral pressure or pull on the tubing. This avoids the need for undue tension on the headgear straps, more comfort and no facial marks.
I also found the vents to be an elegant solution to the problem of noise and the cold stream of air that characterized traditionally vented pillows.
EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
PART 1
THE GOOD
I am recapping an earlier post I made to provide context for this post.
To begin, I would like to say that I love the Airfit P10 for its innovative solution to the problems with the headgear and vents of traditional nasal pillows.
I am a physician and have used well over 20 different products from full face to nasal mask and pillows since being diagnosed with OSA. I finally settled on the Resmed AirSense 10 Autoset and P10 pillows.
I found that its light weight, split head strap resulted in much improved lateral stability over the usual pillow design, which tended to pull upward and back. This was necessary because of the need to provide upward tension against the nostrils. The price was less lateral stability and leaks. This was compensated for with beefier straps for pulling the head gear tighter, resulting in discomfort and the inevitable depression marks on your face. The P10 headgear pulls both upward and downward resulting in force vector more directly backward from the nose while still maintaining a good seal. This creates a four-point restraint that makes the pillow much less prone to being dislodged by any lateral pressure or pull on the tubing. This avoids the need for undue tension on the headgear straps, more comfort and no facial marks.
I also found the vents to be an elegant solution to the problem of noise and the cold stream of air that characterized traditionally vented pillows.
Since I treat patients with anxiety, mood, and bipolar disorder, I know that the quality of their sleep can have profound implications on their symptoms and success of treatment. Since being diagnosed myself, I began to screen very carefully for OSA and have had a large number of patients get diagnosed with OSA. For most of these patients, my number one recommendation for non-mouth breathers is the AirSense 10, teamed with the AirFit P10 (when tolerated).
But now, I have to give them a warning: If you wake feeling short of breath, put the back of your hand (better if licked as moisture increases sensitivity) close to the vents, if your hand doesn’t detect a cool breeze, then your vents could be obstructed. Look to see if there is rainout in the tube.
THE BAD
In 2016, I had discovered a problem after using a P10 for about 6 months. It was now in the winter and the ambient room temperature was cooler. I was using the Resmed insulated jacket for the heated supply hose, with the heater and humidity set in the middle ranges.
I awoke abruptly one night with acute dyspnea (sensation of shortness of breath) and tachypnea (rapid breathing). I immediately thought of hypercapnia and checked for flow from the vents: There was none. On examination, there was slight condensation in the tubing.
While holding the pillows forcefully against my face I exhaled as hard as I could into the pillows. I could feel a fine mist of water hit my hands and then I could feel that the air was exiting the vents again. The vents seemed to clear and I tried to resume sleeping, but I soon awoke with it plugged again.
There was another clue that the vents were obstructed. One night I awoke dyspneic and heard a strange crackling sound in front of me. I realized it was coming from the vents so I put my phone close to them and recorded the sound. This crackling noise was the result of my increased efforts to inhale, which overcame the surface tension of the water covering the “pores” in the vent. But the pores quickly resealed as the crackling persisted with each inhalation and no air was flowing out the vents. Of note, the crackles only occurred on inhalation, not exhalation, meaning there was no flow out the vents even with heightened respiratory effort. You can hear this recording at:
Opening Snaps
I wondered why, after prolonged use I had suddenly experienced complete occlusion of the vents. It had occurred without any warning. So, I searched the Apnea Board Forum to see if others were experiencing a similar problem and was directed to a relevant thread--now 24 pages long!
I read that others were experiencing abrupt blockage of the P10 vents despite an initial period without problems. Some attributed it to moisture trapped in the vent layers, leading some to advocate never cleaning or wetting the vents. Some were resorting to perforating the vents with pin holes or slits. Others kept one in reserve or just gave up on the mask altogether.
Others were dismissive, not believing this could possibly be a problem: Afterall, Resmed is a high-tech medical device company that spends lots on R&D and would never risk the liability of such a design defect. It was FDA approved after all.
Some used leak rates in an attempt to disprove possible vent obstruction. Still others claimed that one could never overcome the pressure of the CPAP fan by rebreathing upstream in the tube and that any increase in CO2 would quickly be flushed out. And some said a person would be forced to awaken by hypercapnia and that the mouth would be the obvious safety valve, preventing any substantial rise in CO2.
AND THE UGLY
But I was certain the obstruction was, in fact, occurring. I decided to find more definitive ways to answer this question. First, I acquired a digital microscope to better understand the nature of the vents. This allowed me to use 60-250x magnification.
This revealed that the vents consisted of tightly woven, layered fibers. I then compared the P10 that had obstructed to a brand new one. The older one appeared slightly grey/brown to the naked eye, but magnification revealed that the old P10 had accumulated very fine deposits of dust particles deep within the interstices of the web. These deposits were visible on both the outer and inner surface of the web. The pattern of the web surface was also different on each side. The inner side seemed to have a tighter pattern of deeper pockets where the dust deposited in bands
I attempted to clean out the deposits with soft brush and soapy wash as suggested in the manual. This did remove a fair bit of more superficial dirt but seemed to leave the deepest deposits. Presumably, these deposits likely accumulate in the areas of greatest airflow and are first to accumulate and hardest to dislodge.
I decided to try something more radical. I filled the P10 tube with soapy water, blocked the pillow outlets and submerged it under water. I then directed blasts of air into the tube from my 100 psi compressor. My thought was this burst of water propelled by a bubble of air would likely distend the web enough to allow for the deposits to wash free. Indeed, the vents were pretty clean after this process. But this was hardly a handy solution for most people.

 EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA--PART 2
At this point I felt I had defined the problem: Use of the P10, even with proper CPAP filter maintenance will eventually lead to fine deposits of dust in the webbing, just as with any filter. While not initially a problem, once critical mass is reached along with rainout conditions, the dust turns to “mud” and effectively occludes the vents.
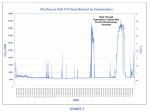
Still, I felt the definitive proof that the vents were truly obstructed and clinically significant would require proof of a measurable increase in CO2 in the tubing.
To this end, in late 2016, I decided to make a capnograph to measure the CO2 within the P10 tubing. I acquired a very sensitive carbon dioxide sensor that could measure 0-20% CO2 at 20 times per second. Unfortunately, the software to support this instrument proved faulty and after waiting 6 months for this to be resolved, I lost interest and moved on to other things.
But in 2018, I was spurred on to renew my efforts with the onset of winter, since I knew that this phenomenon most likely occurred in cooler weather when the P10 was more susceptible to rainout conditions. I also read of additional reports of blocked P10s in the sleep apnea forum in a recent thread started by Hulk, with very inciteful comments by DaveResmedP10 who persevered in pushing back on those who dismissed his concerns:
Rebreathing causing Hypercapnia (CO2 – Carbon Dioxide Poisoning)
I already had all the components for the capnograph:
1 thin anesthesia gas sampling line 6 Nafion dryer tube
2 water trap 7 Air pump
3 particulate filter 8 CO2 sensor and housing
4 hydrophobic filter
It is, however, a simplified instrument, and I don’t suggest it has the precision of a medically approved device. It does respond almost instantaneously to changes in CO2, and I do believe it is sufficiently sensitive for the intended purpose.
Because I wanted to induce the conditions that I suspected caused the obstructions, I used a P10 that was probably 7 months old. I kept the room cool, in the mid to upper sixties. I did not use an insulating jacket on my heated tube, and set the temperature to around 78 degrees and the humidity to 5-6 on the AirSense 10. The intake for the gas sampling was positioned at the junction between the P10 tubing and the supply hose. This level typically was proximal enough from the pillows that, under normal ventilation, the CO2 level was close to ambient room levels. I figured that a substantial rise at this juncture must mean the vents are restrictive enough to result in significant accumulation and rebreathing of CO2.
I believe this capnographic data shows, conclusively, that the P10 vents do, in fact obstruct under conditions where there is a significant degree of residual dust trapped in the vents, as well as moisture from condensation.
The resultant acute rise in CO2 forces the rebreathing of levels approaching end-tidal CO2. I can tell you that after a brief period of hypercapnia I would wake up feeling very short of breath and be breathing rapidly. Sometimes I would just rip the mask off in my sleep. At other times, I awakened and tried to continue breathing in the P10 to see if the obstruction could resolve spontaneously. On a few occasions the vents did reopen, and I then continued to sleep through several subsequent elevations.
In graph 7, I awakened quite dyspneic. But I was determined to keep breathing into the P10 to see what would occur (may not have been the safest thing to do). I had to fight the growing urge to breath more rapidly or to rip the mask off. I began to feel quite unwell. Hard to describe: A feeling of restless anxiety, headache, mild grogginess and slight nausea. Ultimately, I had to abort the test by forcefully blowing into the P10 several times until it reopened. But subsequently, I didn’t feel well for 30-45 minutes and was not able to fall back to sleep for quite some time.
I believe that this data proves the P10 vents can occlude resulting in rebreathing of very high levels of expired CO2. I also believe it dispels the notions that significant hypercapnia would always provoke awakening or that the natural safety valve, namely one’s mouth, would always come to one’s defense.
Finally, as I was reading through Hulk’s recurrent question about where the air was going if it wasn’t going out the vents, I decided it would be useful to actually measure the CO2 inside the intake port of the AirSense 10 to see if there was any evidence that rebreathed air was backing up all the way through the CPAP (see GRAPH 8).
What I found was that, with the vents completely occluded, I could quickly detect a rise CO2. It did not rise way up, going from around 700 PPM to 900-1500 PPM where it reached a steady state. It seemed there was a lot of churn at the port entrance, as I could feel an ebb and flow and the levels would fluctuate if I moved my fingers around the port. Switching the sampling line to the P10 revealed that the CO2 within the tube was over 35,000 PPM. The leak rate did not indicate that the vents were completely obstructed. The only leaking taking place was back out the intake unless there are other leak sites in the CPAP. When the vents are obstructed, it’s actually quite easy to exhale into the CPAP. It almost felt like the resistance I felt before using the EPR. With the vent’s blocked, there is not the same pressure differential from CPAP to the vents.
EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA--PART 2
At this point I felt I had defined the problem: Use of the P10, even with proper CPAP filter maintenance will eventually lead to fine deposits of dust in the webbing, just as with any filter. While not initially a problem, once critical mass is reached along with rainout conditions, the dust turns to “mud” and effectively occludes the vents.
Still, I felt the definitive proof that the vents were truly obstructed and clinically significant would require proof of a measurable increase in CO2 in the tubing.
To this end, in late 2016, I decided to make a capnograph to measure the CO2 within the P10 tubing. I acquired a very sensitive carbon dioxide sensor that could measure 0-20% CO2 at 20 times per second. Unfortunately, the software to support this instrument proved faulty and after waiting 6 months for this to be resolved, I lost interest and moved on to other things.
But in 2018, I was spurred on to renew my efforts with the onset of winter, since I knew that this phenomenon most likely occurred in cooler weather when the P10 was more susceptible to rainout conditions. I also read of additional reports of blocked P10s in the sleep apnea forum in a recent thread started by Hulk, with very inciteful comments by DaveResmedP10 who persevered in pushing back on those who dismissed his concerns:
Rebreathing causing Hypercapnia (CO2 – Carbon Dioxide Poisoning)
I already had all the components for the capnograph:
1 thin anesthesia gas sampling line 6 Nafion dryer tube
2 water trap 7 Air pump
3 particulate filter 8 CO2 sensor and housing
4 hydrophobic filter
It is, however, a simplified instrument, and I don’t suggest it has the precision of a medically approved device. It does respond almost instantaneously to changes in CO2, and I do believe it is sufficiently sensitive for the intended purpose.
Because I wanted to induce the conditions that I suspected caused the obstructions, I used a P10 that was probably 7 months old. I kept the room cool, in the mid to upper sixties. I did not use an insulating jacket on my heated tube, and set the temperature to around 78 degrees and the humidity to 5-6 on the AirSense 10. The intake for the gas sampling was positioned at the junction between the P10 tubing and the supply hose. This level typically was proximal enough from the pillows that, under normal ventilation, the CO2 level was close to ambient room levels. I figured that a substantial rise at this juncture must mean the vents are restrictive enough to result in significant accumulation and rebreathing of CO2.
I believe this capnographic data shows, conclusively, that the P10 vents do, in fact obstruct under conditions where there is a significant degree of residual dust trapped in the vents, as well as moisture from condensation.
The resultant acute rise in CO2 forces the rebreathing of levels approaching end-tidal CO2. I can tell you that after a brief period of hypercapnia I would wake up feeling very short of breath and be breathing rapidly. Sometimes I would just rip the mask off in my sleep. At other times, I awakened and tried to continue breathing in the P10 to see if the obstruction could resolve spontaneously. On a few occasions the vents did reopen, and I then continued to sleep through several subsequent elevations.
In graph 7, I awakened quite dyspneic. But I was determined to keep breathing into the P10 to see what would occur (may not have been the safest thing to do). I had to fight the growing urge to breath more rapidly or to rip the mask off. I began to feel quite unwell. Hard to describe: A feeling of restless anxiety, headache, mild grogginess and slight nausea. Ultimately, I had to abort the test by forcefully blowing into the P10 several times until it reopened. But subsequently, I didn’t feel well for 30-45 minutes and was not able to fall back to sleep for quite some time.
I believe that this data proves the P10 vents can occlude resulting in rebreathing of very high levels of expired CO2. I also believe it dispels the notions that significant hypercapnia would always provoke awakening or that the natural safety valve, namely one’s mouth, would always come to one’s defense.
Finally, as I was reading through Hulk’s recurrent question about where the air was going if it wasn’t going out the vents, I decided it would be useful to actually measure the CO2 inside the intake port of the AirSense 10 to see if there was any evidence that rebreathed air was backing up all the way through the CPAP (see GRAPH 8).
What I found was that, with the vents completely occluded, I could quickly detect a rise CO2. It did not rise way up, going from around 700 PPM to 900-1500 PPM where it reached a steady state. It seemed there was a lot of churn at the port entrance, as I could feel an ebb and flow and the levels would fluctuate if I moved my fingers around the port. Switching the sampling line to the P10 revealed that the CO2 within the tube was over 35,000 PPM. The leak rate did not indicate that the vents were completely obstructed. The only leaking taking place was back out the intake unless there are other leak sites in the CPAP. When the vents are obstructed, it’s actually quite easy to exhale into the CPAP. It almost felt like the resistance I felt before using the EPR. With the vent’s blocked, there is not the same pressure differential from CPAP to the vents.


RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
mdmarmd, that is some very compelling evidence of the CO2 increase within the P10 breathing space. Have you tried to submit this data to Resmed?
I will bookmark this thread for publication as an Apnea Board wiki article. I assume you approve of that. If you want author credit, please feel free to contact me by PM.
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
SleepyRider
That's OK but I need you to fix some things:
The two pictures at the top are in the wrong place. And I was trying to post two more parts and they got lost somewhere.
Doug
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
This is very interesting. I am curious if this is related to mask design or is it inherent to the mask style. Do you have another pillow style mask, like the F&P Brevida, to run the CO2 tests on for comparison?
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
Crimson Nap,
I tried to post a reply but it got lost in the ether as did parts 3 & 4 of my original post.
I think all apparatus probably have some CO2 retention due to restriction on flushing. But I think these diffuser types, though very nice, are particularly susceptible due to the very high degree of restriction to flow they cause. I think the flow dynamics of these, especially as they are highly turbulent, are much trickier to perfect than simple hole type vents.
I did make a hybrid pillow from a P10 + Nuance. I tried to post this picture on Part 3 but it got lost somewhere. I did test it and it did raise CO2 but not to the level the P10 reached.
[attachment=10444]
I have a bunch of different masks, from pillows, to nasal and full face masks. But I can’t test anymore at this time. I completely messed up my house—bedroom, and family room—and my wife is going crazy.
Also, test nights are very disruptive. The air pump is noisy, my lap top is next to my bed and the hypercapnic episodes wake me up and I feel sick the next day, so I have to restrict it to nights where I don’t work the next day.
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
Sometimes a designed "enhanced expiratory rebreathing space" (EERS) is desirable. Here is an article I did earlier last year. http://www.apneaboard.com/wiki/index.php...ace_(EERS)
02-24-2019, 11:29 PM
(This post was last modified: 02-24-2019, 11:58 PM by mdmarmd.)
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
I am reposting Part 3 & 4 which got lost in the ether. I wanted them to be reasonably close to the original post.
I now cannot make anymore attachments for some reason so I am resorting to pasting the URLs in for the pictures (when I used the "insert image" option the pictures were always broken for some reason.
EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
PART 3
EPILOGUE:
I believe the AirFit P10 is a very innovative nasal pillow. However, in certain conditions, mainly when there is sufficient accumulated dust mixed with condensation, the vents may entirely obstruct leading to acute hypercapnia.
This could be a significant risk for those who sleep through these events, especially if they have concomitant medical conditions such as COPD, (Overlap Syndrome: COPD + OSA) where hypercapnia and compensatory acidosis already pose risks. Other medical conditions such as CHF, and cardiac arrhythmias (AF, V-Tach, Bradycardia), might also be vulnerable to hypercapnia. In people prone to anxiety, elevated CO2 is known to provoke panic attacks.
Interestingly, studies in submariners and astronauts suggest that chronic exposure to even lower levels of CO2 may affect calcium metabolism and deposition, bone resorption and potentially renal injury from abnormal Ca+ and serum pH. Pulmonary and cerebral artery flow is also increased.
I found one paper that concluded: “Hypercapnia is a key correlate of EEG activation and daytime sleepiness in hypercapnic SDB (sleep disordered breathing) patients. The relationship between hypercapnia and sleepiness may be mediated by reduced neuro-electrical brain activity. (https://www.ncbi.nlm.nih.gov/pmc/article....5.517.pdf)
An additional concern is that if one suffers hypercapnia and pulls the pillows off while asleep, the groggy, headachy feeling experienced the next day may easily be attributed to hypoxemic apnea events rather than CO2 toxicity. In fact, both may be occurring. Some doctors, unaware of this risk could easily attrri
The Resmed Airfit P10 user manual instructs and warns:
GENERAL WARNINGS
· The vent must be kept clear.
· The mask should only be used with CPAP or bilevel
devices recommended by a physician or
respiratory therapist.
· The mask should not be used unless the device is
turned on.
Once the mask is fitted, ensure
the device is blowing air.
Explanation: CPAP and bilevel devices are intended to be used with special masks (or connectors) which have vent holes to allow continuous flow of air out of the mask. When the device is turned on and functioning properly, new air from the device flushes the exhaled air out through the mask vent holes. However, when the device is not operating, insufficient fresh air will be provided through the mask, and the exhaled air may be rebreathed. Rebreathing of exhaled air for longer than several minutes can, in some circumstances, lead to suffocation.
· As with all masks, some rebreathing may occur at
low CPAP pressures.
WARNING
Always follow cleaning instructions and use mild soap. Some cleaning products may damage the mask, its parts and their function, or leave harmful residual vapours that could be inhaled if not rinsed thoroughly.
CAUTION
· If any visible deterioration of a system component is
apparent (cracking, crazing, tears etc),
the component should be discarded and replaced.
Daily/After each use:
· Disassemble the pillows from the frame according to
the disassembly instructions.
· Thoroughly clean the separated mask components
(excluding headgear), by gently rubbing in
warm (approximately 30°C) water using mild soap.
· To optimise the mask seal, facial oils should be
removed from the pillows after use.
· Use a soft bristle brush to clean the vent. Inspect
each component and, if required, repeat
washing until visually clean.
· Rinse all components well with drinking quality
water and allow to air dry out of direct sunlight.
Dry the vent by gently wiping with a cloth.
· When all components including the vent are dry,
reassemble according to the reassembly
instructions.
Problem/possible cause Solution
Vent is blocked or dirty/discolored.
If the vent requires cleaning, use a soft bristle brush. The vent may discolor over time and this is not a safety concern. Follow the cleaning instructions in this guide to maintain performance and safety of the mask.
Vent is wet. Ensure the vent is dry after cleaning and in the case of excess condensation.
Technical specifications
The mask contains passive venting to protect against rebreathing. As a result of manufacturing variations, the vent flow rate may vary.
These instructions underscore the critical importance of the vents remaining unobstructed, yet they are deficient in several respects:
· The vents can obstruct under usual operating
conditions.
· You can’t easily see if the vents are clean with
the naked eye.
· Discolored vents are not inconsequential, and
may, in fact, be the only sign of an
impending health risks.
The best way of resolving this potential risk to health would be for Resmed to redesign the vents so that there is slightly more air flow, thus allowing for less potential for trapping dust. This would also facilitate dislodging such deposits with usual cleaning. I don’t have any idea how difficult an engineering problem this poses. I know that you need a rather high degree of obstruction before you substantially reduce blood flow, say in a coronary artery. It’s possible that the tolerance for the inter fiber spaces needs to be quite tight and the laws governing turbulent air flow may be quite complex. But presumably some redesign of the vents would permit more flow without defeating the benefits.
But whether the company would be responsive to such a need is another question. This problem has been identified now for at least four to five years and some have reported on the forum that when they have voiced concerns with the company, they have been dismissed. DaveResmedP10 wrote on the forum:
“I have contacted the retailer and Resmed about it mostly to ask if it could be a manufacturing fault because the vast majority of comment online is all good. Resmed say 'no such problem exists, never had a manufacturing fault, you need to get used to it or change masks'. The retailer had heard of the issue and said some people believed that it was due to washing the mesh in hot water causing it to close up.”
At the very least, I think the user manual needs to have “a black box warning” alerting users to the potential risk of rebreathing and how to detect it.
Barring any design change, what can be done by those who still prefer using the P10 to minimize the risk of hypercapnia? I would make the following suggestions:
· Make sure that you keep changing your CPAP filter
regularly. Don’t wait until it has a significant layer of
grey dust over it. (I recall reading a post that
questioned why one needs to use a filter on the
CPAP. The response was it retards the
accumulation of dust on the blower blades. In this
instance, it serves a much more
critical function.)
· Wash your vents regularly and visually inspect them
carefully. (Make sure to press something
white like tissue paper behind the inner surface of
the vent during your inspection as this
accentuates the appearance of accumulated dust.)
When they begin to look slightly darker or
grey/brown compared to a new P10, be aware that
they might occlude if there is condensation and may
need to be replaced.
· Try to minimize conditions that promote
condensation, especially during colder weather;
adjust ambient temperature, use a heated supply
line and a warming jacket. However, I have
experienced occlusion even when there is barely
detectable condensation.
· Consider avoiding the use of the Expiratory
Pressure Reduction feature in conditions when
the risk of condensation is greater since a reduction
in average pressure might reduce
ventilation of CO2, and increase the risk of vent
occlusion
· Frequent replacement of the frame may be
necessary, particularly if you live in a dusty
environment.
· Remember: Some members have reported
obstructed vents with NEW P10's so in certain
circumstances, condensation alone may be
sufficient to cause occlusion
While some insurances may replace the frame fairly frequently, others may not and users may face a significant cost to buy them outright. (One member posted: BTW, I don't get new ones - I have to buy new ones and this mask retails in Australia for $275.) For these, I would recommend a method of cleaning beyond simple soap/brushings. Contrary to some advice, I would not suggest never washing your frame.
I can recommend an alternative method of cleaning the vents: I cut the ends off a standard CPAP hose (the kind with the thick grey rubber connectors) leaving an inch or two of tubing attached to each connector. Find a tube with a diameter close to the internal diameter of the tube and use it to connect the tubes together with silicon.
This can now be used as adaptor to fit over a standard faucet aerator. (If you have a flared faucet you will have to make an appropriate adaptor). I considered just sticking it on the end of a garden hose nozzle. But I preferred to use warm water from the sink as I think it may facilitate a more thorough cleansing.
I molded a silicon plug to close off the pillow openings and attached the pillow to the frame. I put a bunch of liquid soap in the tube, attach it to the faucet and then run fairly warm water through it for 10-20 minutes. Turn it as high as you can without blowing it off the faucet. This process cleaned the vents as well as the 100 psi air blowout did and is certainly more practical.
Conveniently, this plugged pillow can also be stuck onto your P10 frame, and once you get the blower started connect your P10 tube to the supply hose. This will provide sufficient resistance to keep the blower running and force air out the vents to dry them out.
I had read somewhere in forum threads that some had used an ultrasonic cleaner to clean their P10. I didn’t have one, but I thought my cleaning recommendations wouldn’t be complete without a trial with this so I purchased one.
To my great disappointment, after 480 seconds in the cleaner there was no appreciable improvement in the amount of debris ensconced in the P10 vents. I actually only submerged one vent and left the other out of the water so I could make a direct comparison.
Visually and microscopically they both looked the same after the “cleaning”. And the water, looked completely clear after the process. In comparison, when I did my watch, the water became visibly cloudy with grunge from the watch band. This suggest to me how hard it is to remove the deposits with just brushing.
As a last resort, if you really like the P10, it’s head gear and pillows, but don’t want to contend with the risk and inconvenience of the occasional obstruction, you can consider making a hybrid that keeps most of the benefits of the P10, minus the vents, but adds the convenience of a swivel.
I had tried a Respironics Nuance before and noticed that it’s shape, when carefully carved up, could be neatly attached to a P10 frame whose hose was removed.
I easily attached the two using Loctite GO2, a somewhat rubbery clear glue (It did yellow over time). I now use this as a spare, especially when I go somewhere like my RV where I have less control over the ambient temperature. It’s comforting to know that I won’t be stuck, unable to use a wet P10 for the rest of the night.
FAUCET JET ADAPTER
https://photos.google.com/share/AF1QipNuhTifr1ExcrTTWHNC5PlZF0p5RigvveF7UiExyiSuyC_BvIpG8__qv6Osx7HWYw/photo/AF1QipMdDuqqVUwHeVvFYj8jfWellmU6wZluIkiuJ7U6?key=ZEpJbGY5R0luQnJ3aGFHVGN6OUlnaHpCei1zUkZB
https://photos.google.com/share/AF1QipNuhTifr1ExcrTTWHNC5PlZF0p5RigvveF7UiExyiSuyC_BvIpG8__qv6Osx7HWYw/photo/AF1QipMoReBoIGp9xSXgtA2wVll0f3sotOCQYwscWWew?key=ZEpJbGY5R0luQnJ3aGFHVGN6OUlnaHpCei1zUkZB
HYBRID P10 + NUANCE
https://photos.google.com/share/AF1QipNu...pCei1zUkZB
ADDENDUM:
Initially I had difficulty finding data on the medical and physiologic risks at various levels of CO2. I found charts that showed symptoms up to 40,000-50,000 PPM but then there was uncertainly across a big spread from 40,000 PPM to 100,000 PPM (the latter being quickly be lethal).
I have since found some charts that give more precision to the risks as the levels continue to increase. It appears the levels achieved in my experiments clearly presented potential risks to one’s health.
I realize now, that it was probably unwise for me to continue to re-breath the clearly elevated CO2 in my tests, but I saw that I had clearly been exposed to levels in the 40,00-45-000 range and figured a lot of other P10 users had as well: Still, probably not the best idea.
Toxicologist, Susan A. Rice, Ph.D., D.A.B.T. has a very interesting web page that shows detailed effects of elevated CO2 in both acute and chronic exposure and in susceptible populations such as those with medical conditions and those using certain medications or alcohol.
If you are interested, you can find this at:
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.464.2827&rep=rep1&type=pdf
To give some context, I have included some charts that indicate levels and potential health problems at progressively higher levels of CO2:
Carbon Dioxide – Physiologic Effects
Volume Carbon Likely Effects
Dioxide In Air
1-1.5 % Slight effects on chemical metabolism after
exposures for several hours
3 % The gas is weakly narcotic as this level,
giving rise to deeper breathing, reduced
hearing ability, coupled with headaches, an
increase in blood pressure and pulse rate
4-5 % Stimulation of the respiratory center occurs
resulting in deeper and more rapid breathing,
signs of intoxication will become more
evident after 30 minutes exposure
5-10 % Breathing become more laborious with
headaches and loss of judgement
10-100 % When the carbon dioxide concentration
increases above 10%, unconsciousness will
occur in under one minute and unless prompt
action is taken, further exposure to these high
levels will eventually result in death.
CARBON DIOXIDE--PROGRESSIVE RISK CHART
https://photos.google.com/share/AF1QipNu...pCei1zUkZB
CARBON DIOXIDE EXPOSURE STANDARDS AND EFFECTS PART 1
https://photos.google.com/share/AF1QipNu...pCei1zUkZB
CARBON DIOXIDE EXPOSURE STANDARDS AND EFFECTS PART 2
https://photos.google.com/share/AF1QipNu...pCei1zUkZB
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
REPOSTING LARGER PICTURE OF GRAPH 8 AS IT WAS TOO SMALL TO READ
https://photos.google.com/photo/AF1QipOC...IXoeU6iwhy
RE: EVIDENCE OF AIRFIT P10 VENT OBSTRUCTION CAUSING HYPERCAPNIA
(02-25-2019, 12:20 AM)mdmarmd Wrote: REPOSTING LARGER PICTURE OF GRAPH 8 AS IT WAS TOO SMALL TO READ
https://photos.google.com/photo/AF1QipOC...IXoeU6iwhy
mdmarmd-
Thanks for sharing the research you have conducted. It seems a little scary to be using an Airfit p10 right now which is what I was given with my new Resmed Airsense 10 Autoset less than a week ago. I also was given an F&P Eson2 during my one week titration period with a loaner Resmed Airsense 10 Autoset machine.
What would you recommend to someone who is currently using the p10, new or otherwise? I can revert to the Eson2 and/or perhaps get a replacement through Kaiser for my Airfit p10. It's rather interesting that while trying to correct one health malady, sleep apnea, another may rise up due to the risk of CO2.
Thanks very much for any advice you could give me on this!
|








