Optimizing therapy
First and foremost, help is readily available at our forums. Please feel free to ask any questions about your apnea there. Please keep your posts in one thread to maintain history.
It is impossible to advise on a cause or a correction without knowing the types of events and what your Autoset machine is doing in terms of pressure. This is a long and drawn out way of saying We Need To See The Data.
Contents
- 1 APAP Optimization / Titration
- 2 CPAP titration
- 3 BiPAP/BiLevel Titration Protocol
- 4 ASV Titration Protocol
- 5 TroubleShooting Therapy
- 6 Obstructive Apnea (OA)
- 7 Complex or Mixed Apnea (OA / CA)
- 8 Central Apnea (CA)
- 9 EPR
- 10 Other Software
- 11 Tips and Tricks
- 12 What Not To Do
- 13 Principiles and Terms of Titration
- 14 DISCLAIMER & LEGAL NOTICE
APAP Optimization / Titration
APAP is an effective treatment for moderate to severe obstructive sleep apnea with variable automatic pressure.
There are two parts of Optimization, The first is the numbers which we discuss below. Also of great importance is how you feel. This is very subjective. Please do not ignore this aspect of your optimization and ask for help on our forums.
Step 1: Review your sleep Studies Review your initial (or recent) Sleep Study, this is the one done without a xPAP machine. In this study you are wired to measure your sleep stage (EEG) and cardiac function EKG, Are you mouth or nose breathing, and your O2 Saturation levels thru the night. This study determines the proportions and types of Apnea that you experience including the non-obstructive apneas which are more complex to treat. For us here it determines the presence or absence of Central and / or Complex Apneas.
Review your (typically) second study, your titration study. This is where a pressure recommendation is made. This recommendation is a good starting point but it is a single point in time where you are sleeping in an unfamiliar bed in an unfamiliar location with a bunch of wires stuck to your head and various other straps and monitors.
A Caution flag. If you have Complex or Central Apnea (CA) make only small changes and see how they impact your data. Obstructive Apnea is generally treated by increasing pressure. Central Apnea often increases with an increase of pressure. These two treatments (decreasing pressure for Central Apnea and increasing pressure for Obstructive Apnea) often contradict each other. It’s possible one or other of the sleep studies (ie diagnostic and titration) may be skipped. In this case carefully monitor your results to see if you have central apneas. Some machines and software refer to these as clear airway events – a subtle but important distinction.
Step 2: Your Machine OK, now we can get down to the nitty gritty, your machine. While there are excellent used and new older model machines out there, we will concentrate on the new current machines here. If cost and payment indicate otherwise please enquire on the forum for choices. The best machine to get is the current Auto Machine, currently Philips Respironics DreamStation Auto or the ResMed AirSense 10 (A10) AutoSet There are other specialized PAP machines, BiPAP, BiLevel, ASV etc. that this article is not intending to discuss. Please visit our forums for questions involving these machines. A recent recommendation on the forum was “Get the auto, request the Resmed Airsense 10 Autoset as the machine you want, and you will be on your way in no time.” If you do not have an Auto machine as above optimization can be achieved if you have a full data capable machine. For access to the widest range of on-line assistance, your machine should be compatible with the OSCAR software, but having full data capability and access to the Vendors software will also work. If your machine only offers AHI data, while certainly not optimal, treatment can be somewhat optimized by the trial and error method sometimes called educated guesses. Please request help on our forums for this.
- Getting Your Machine
- If you are buying your own machine purchase one of the above machines or inquire on the forums for a used or other alternative to purchase.
- You have the most power on getting the right machine by knowing what you want to get and expressing this to both your doctor and your DME BEFORE you have agreed to receive/pay for it
- Realize three things
- It is YOUR therapy.
- It is YOUR money, you are paying for it either with insurance money, deductibles, or your own money.
- YOUR most leverage occurs before you actually purchase/rent your machine.
- Most DMEs {Durable Medical Equipment Suppliers) have a financial interest in the transaction, which pays them the same whether a basic "brick" or a premium full-efficacy data machine is dispensed. Meeting the minimum requirement of the prescription is the only mandate for a DME, and the uninformed patient who goes in to receive a machine will receive the machine that best serves the DME (financially), while meeting the minimum requirements of the prescription. Data is important. You should control your own therapy, and most suppliers fail to help you to do this. The "trained health care specialists" are constrained by the prescription from a short and as such, typically inaccurate sleep study, titration study, or the default settings of an auto machine.
- If your Sleep Study shows a lot of Central Apnea, or you have a respiratory disease (CHF, COPD, etc.) please post this info on the forum and ask for advice. This generally indicates the need for a "BiLevel ASV machine. This is a highly specialized and as such expensive machine.
Step 3: Download and install the OSCAR software
Once OSCAR is installed on your computer, insert the SD card from your machine into the computer and allow OSCAR to import the data and display your results. Please see the OSCAR Help page for more information.
Step 4: Initial Pressure Setting
If your doctor or DME has not already set the pressure, or you do not have a prescribed pressure, then set the APAP machine for 6-20 cmH2O in Auto mode. – This is to get the first look at what the machine will use.
If you have data because you have been using CPAP evaluate the chart data,
The pressure should only go up as high as needed to resolve events and flow limits. Some people do need a maximum pressure defined to prevent the machine from going excessively high. This value, the maximum pressure, will be set on the second night if desired.
Step 5: Upload the Data Create a screenshot of your OSCAR output and upload it to the forum and ask for an evaluation. Please keep all of your posts in a single thread to maintain history. Guidance on downloading, organizing / formatting the OSCAR output, and attaching it can be found below:
Please note: not all charts are important
What are we looking for? First we look for anything that may present issues with managing your therapy, This includes any sign of CA, Central Apnea or Complex Apnea. If there are any signs we will proceed cautiously.
What is the relationship between your assigned pressure range and your running range? Are you hitting the high number and staying there? Are you sitting on the bottom or low number. The low number, the EPAP provides the support for OA, Obstructive Apnea and Hypopnea. We are also looking for relationships between Events and the various charts that OSCAR presents.
Step 6: Analyze the Data
- 6.1 Maximum pressure
If the machine reaches the maximum set pressure and stays there for a period of time, this indicates that it is trying to go higher to treat obstructive events. (This applies if your maximum pressure is less than 20. If it is set to 20 and the machine is stuck there, a more detailed analysis is necessary, and a different type of machine may be required). Frequently we see pressure induced CA events. We want to minimize these so we will lower Max Pressure as necessary to accomplish this frequently ending with a very narrow pressure range or even a single fixed pressure.
- 6.2 Minimum pressure
If your pressure is too low you are likely to see obstructive apneas and hypopneas. If you notice your average auto pressure is higher than your minimum setting, the hypopnea are likely from the minimum pressure being too low. A good rule of thumb is to keep your minimum pressure setting about 2-cm below your 90% pressure (PR) or Med Pressure (ResMed) or near the average if they are close. The Dreamstation tends to be conservative with raising pressure, and the algorithm favors returning to the minimum setting. This can often adequately treat OA, but leave you with excessive Hypopnea (H) events. The remedy is an increase in the minimum pressure setting. PR machine: If your 90% setting is 12 cmH2O Min is set to 10 cmH2O and Max Remains at 20 cmH2O ResMed machine: Use the Med value for pressure. If your Med setting is 11 cmH2O, set the minimum to 9 cmH2O and Max remains at 20 cmH2O. Note: there is no need to reduce the max unless there is concern over CA events or to minimize the max for comfort at this time. Note that once your titration is complete a good practice is to set the max pressure for just above the max that you normally see, just to prevent “run-away” pressures and leave enough room that you can see your pressure ran higher than you expected.
Step 7: Repeat Conditions change. Perhaps you have gained some weight, (I KNOW that has NEVER happened to any of us (sarcastic switch off)), or you are now sleeping on your right side instead of your left, or you have a new pillow. It doesn’t matter what, but things change. And when these conditions change your apnea may or may not be impacted.
- Note:
It is the exhale pressure that needs to be elevated to prevent Obstructive Apnea (OA), and it is the pressure differential between inhale and exhale that helps relieve hypopnea.
When your treatment effectiveness may be impacted, when your AHI is higher than expected over a period of time, it is time to re-evaluate your therapy. What do you need to do to positively impact your therapy?
CPAP titration
CPAP is an effective treatment for moderate to severe obstructive sleep apnea with fixed pressure.
- Set your initial pressure, protocols call for values from 4 to 6 or 2-3 cmH2O below your current settings then
- Increase CPAP ≥1 cm H2O every ≥5 mins for obstructive apneas, hypopneas, RERAs and at least 3 min of loud or unambiguous snoring
- Is the patient having obstructive events? If yes, repeat step 2
Obviously we cannot make an evaluation every 5 minutes while we are sleeping so we perform our evaluations in nightly cycles.
Note: By protocol, Titration of 15 cmH2O or greater is justification to go to a BiPAP / BiLevel machine.
ResMed S9 VPAP Tx Sleep Lab Titration User Guide
Including
CPAP and AutoSet Therapy Titration Protocol
VPAP S Therapy Titration Protocol
VPAP ST Therapy Titration Protocol
iVAPS Therapy Titration Protocol
VPAP Adapt Therapy Titration Protocol (ASV)
Philips-Respironics Titration Protocol Reference Guide
Including
CPAP
auto CPAP
BiPAP S
BiPAP Auto
BiPAP autoSV Advanced
BiPAP S/T
BiPAP AVAPS
BiPAP/BiLevel Titration Protocol
The BiPAP/BiLevel machine is ideal for sleep apnea patients who find it difficult to adjust to therapy on a continuous fixed-pressure machine.
Fixed BiPAP/BiLevel Titration
ASV Titration Protocol
ASV / ADAPTIVE SERVO-VENTILATOR
A bilevel device for central breathing disorders such as Cheyne-Stokes respiration, central sleep apnea, or obstructive events.
The Typical Path to ASV
- Try CPAP and Fail
- Try BiPAP/BiLevel and Fail
- Assess if you should be considered for ASV
- Titrate for ASV
- ASV therapy is contraindicated in patients with chronic, symptomatic heart failure (NYHA 2-4) with reduced left ventricular ejection fraction (LVEF ≤ 45%) and moderate to severe predominant central sleep apnea.
The ASV titration protocol is very straightforward, and starts new users on ASVauto mode at 4.0 min to 15 max EPAP, and PS 3.0 minimum to 15 maximum. That is a good starting place, but many users find the pressure can become too much. Most find a PS max of 12 is sufficient to cause breathing during centrals and hypopnea, and can fine-tune EPAP based on the first few days of experience. Many new users start with EPAP min 5.0 if they know they need the airway support against obstructive apnea.
TroubleShooting Therapy
Flow Limitations on non-invasive ventilation including ST, AVAPS and ASV
False Flow Indications
Flow limitation is a common characteristic of pressure support induced inspiration. When you don't make the spontaneous effort to breathe, the ASV pressure support does ensure a volume of air is inspired; however as the lung fills, resistance increases, and this gives the appearance of flow limitation. This is not upper airway resistance, but a function of resistance in the lung itself. We see this on nearly every individual that has posted close-ups of the respiratory flow wave during ASV and ST non-invasive ventilation intervention. We don't try to treat this form of flow limitation, but rather accept that it is a common result of non-invasive ventilation.
The check for whether flow limitation is upper airway or a result of ventilation is to look at pressure support when it occurs. If the flow limitation mostly occurs during higher pressure support, it is pulmonary. If the flow limitation occurs during minimum or low pressure support, it may be upper respiratory, and a higher minimum pressure support or higher minimum EPAP may help.
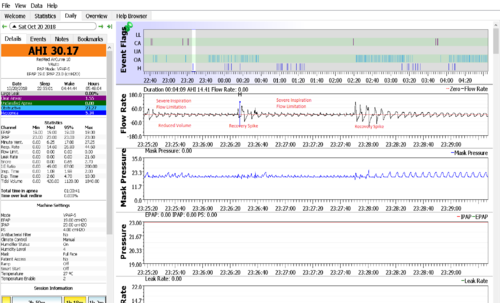
Flow limitation is something that is frequently seen in patients with CA. This chart shows the classic flow limitation profile on an ST, most often associated with a restricted or obstructed airway. There appears to be respiratory effort, but the airflow slows significantly after initiation, and the rate of flow continues to slow until you cycle to expiration. In this sequence, flow continues to diminish until the patient arouses and has recovery breathing.
In this case, looks may be deceiving. Since ST is being used, the machine follows a weak spontaneous effort, but since the patient is not expending enough effort to permit a full breath, the ST is not providing enough pressure support to compensate for the lack of effort. So the airway is open, and with too little pressure support, a flow limited breath occurs that "looks" like restriction. The ASV would have increased pressure support by as much as 15 cm (21/7) instead of the constant 11.6/6.6 pressure the ST provides. That is the "adaptive" part of ASV. If that pressure support boost failed to cause a full breath, then in ASVauto, EPAP would increase to clear obstruction.
The ST is designed for chronic obstructive pulmonary disease (COPD) and uses pressure support to overcome the restricted airway or lung on every breath. It is typically set at PS more than 8.0 cm to do this. The backup rate will then provide a breath in the event of a central event, but the machine is doing most of the work of respiration on every breath in its intended application. It cannot supplement or provide a breath at constant PS 5.0. So what we are looking at is the inadequate flow induced by the ST, not an obstructive flow limitation. With central apnea, you only want to rely on the ventilator when it is needed, and rely on spontaneous effort with low, or no pressure support. This provides a normal respiration for the idiopathic CA patient, whom is adversely affected by constant high PS. If PS is raised to where the machine can compensate for the CA, the patient will be nearly 100% reliant on the machine, because pressure support suppresses respiratory drive in people with CA.
Positional Apnea
Only doctors and therapist think "positional" apnea means supine. We know it is really a chin tuck in any position. It happens a lot on your back because we like to rest our heads on pillows that facilitate chin-tuck, but we have seen positional apnea in any position and even while using so-called "ergonomic" or cervical support pillows. So the professionals erroneously attribute to gravity, what is really just a body position many people naturally have. The simple way to prove this is to sit comfortably in a chair and relax. As you relax further let your chin drop towards your chest. People prone to this obstruction will sense more airway restriction, a snore or even complete apnea. This happens naturally during sleep, even sleeping on your side in a "fetal" position.
If it had not been a factor in at least 1/3 of the members of the Apnea Board Forum, we would quickly dismiss it, but the results are amazing. We have seen some members go from AHI over 30 to less than one without changing any CPAP settings, but adding a soft collar. Someday, even the medical community is going to capitalize on this and start measuring patients for collars, but for now you can DIY for less than $20.
The airway obstruction or positional apnea from chin tucking is more acute when nasal breathing and is typically overcome through arousal and/or mouth breathing. This mechanism of positional apnea appears to affect the same tissue set as palatal prolapse but in a different way. Palatal prolapse/collapse occurs during exhale as the palate prolapses upward into the velopharynx during expiration. In "positional apnea" the theory has been that the back of the tongue collapses into the airway at the same location, restricting the airway. With the chin-tuck theory, the soft tissues under the jaw are pressed upward causing a restriction or collapse during inspiration. It takes very little pressure to make this happen and the negative pressure of the airway during inspiration increases the restriction. You can simulate the chin tuck by pressing lightly upward on the tissues at the back of the lower jaw. Relatively light pressure on this tissue creates an increasing flow limitation ultimately resulting in a series of apneas. The series of apneas causes an arousal that either corrects the airway and/or causes mouth breathing.
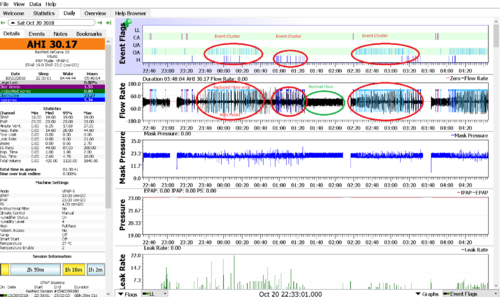
Positional Apnea is caused by misalignment of the airway typically tucking the chin down.
It is normally detected by clusters of Obstructive and Hypopnea events usually associated with an uneven and smaller/narrower Flow Rate chart.
The Flow Rate chart below is scaled to show individual breaths including extremely small Flow Limited breaths
With Soft Cervical Collar
Starting in 2016 we started seeing CPAP users using a loose fitting soft cervical collar (loose fitting because we want comfort and are not stabilizing the neck) to manage Mouth Breathing. Additionally, it was noted to resolve Position Apnea.
Two ways to check for this Positional Apnea
- Sit relaxed in a chair and as you fully relax let your chin drop to your chest and note the increased airway resistance that may range from an increased effort to a snore or full blockage.
- Another test is to gently push upward on the soft part of your jaw or neck right in front of the throat.
If your airway easily closes from that pressure, positional therapy in the form of a soft cervical collar or wedge may significantly improve your results. </br>
The fit needs to support the jaw and chin, without impinging on the throat or soft tissue between the chin and throat. Getting the right fit in terms of height, circumference and feel may take some persistence, but it might also make it possible for you to control OA and H events at lower pressures.
An Anti-Snoring collar (no back) also works as does a CPAP Pillow, or even a small pillow set under the chin, with the pillows being less effective than the collars.
Sometimes the solution is simple, use a smaller pillow to reduce the chin tuck.
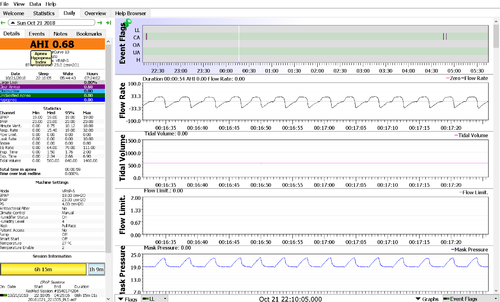
Below is a closeup showing individual breaths in the Flow Rate chart without Flow Limits thanks to the use of a Soft Cervical Collar.
Clear Airway Clusters
At least in this image, we see CA events are highly clustered and that after the first pause in breathing that is not even flagged, you get into a kind of feedback loop of CA followed by recovery breathing (larger flow and volume than normal), and the cycle repeats, and slowly decreases becoming variable or periodic breathing before normal respiration is seen at the end. It's a very interesting sequence, that we have seen before. We think what happens is that following the first pause, you take a large recovery breath which may lower your serum CO2 (HCO3) casing minor hypocapnea which reduces respiratory drive. We can see flow diminishes then suddenly increases as HCO3 increases and spikes your respiratory drive resulting in more recovery breathing that terminates in a full CA event. This is a feedback loop that begins with a minor non-event but then amplifies through the sequence. At the end of the cluster your respiration rate increases to more breaths per minute of smaller flow and goes through several oscillations before normalizing.
This pattern can be exacerbated by pressure support or EPR which tends to increase ventilation to where the apneic threshold is reached. Reducing EPR or pressure support may help to make this feedback loop less likely to occur or eliminate it altogether. You are using fixed pressure of 13.4 with EPR at 3 which is a bilevel pressure of 13.4/10.4. There is nothing wrong with your respiration or neurology, this is just a high sensitivity to increases or decreases of CO2 which directly impacts your respiratory drive (apneic threshold). I think if you reduce EPR you can also lower the pressure by the same amount (12.4 with EPR 2). These events may appear disturbing to see until you understand them and realize they are not particularly harmful to your health or sleep. You may choose to ignore this unless it is a common occurrence or happens fairly often or for longer periods of time.
RERA
RERA Rule for Adults
If electing to score respiratory effort-related arousals RERA, score a respiratory event as a RERA if there is a sequence of breaths lasting at least 10 seconds characterized by increasing respiratory effort or by flattening of the inspiratory portion of the nasal pressure (diagnostic study) or PAP device flow (titration study) waveform leading to arousal from sleep when the sequence of breaths does not meet criteria for an apnea or hypopnea.
Here is how a RERA presents itself in a Detailed or Expanded view.

Where do you look? Where Flow Limit Spikes are always a good idea. Look for the pattern, the flow limit spike is not a requirement, it is only an indicator
Note: Not all machines have a Flow Limit Chart to help. The only way to catch them all is to manually scan using a 2-minute view and the arrow keys looking for the RERA pattern.
Palatal Prolapse
In some individuals with obstructive sleep apnoea (OSA), the palate prolapses into the velopharynx during expiration, limiting airflow through the nose or shunting it out of the mouth.
Symptoms
- palate closing on exhale
- Throat closes during exhale
- Cannot exhale thru nose
Obstructive Apnea (OA)
A good rule of thumb is to keep your minimum pressure setting about 2-cm below your 90% pressure or near the average if they are close. The goal is to raise support (Min Pressure / IPAP) to reduce/minimize/if we are lucky, eliminate Obstructive events. These include Hyponeas, Flow Limits, and Snores. The Max Pressure / EPAP is lowered to minimize other issues (Aerophagia , swallow too much air, too much pressure causes wakeups) if needed. Typically it is set at either MAX pressure (20 cmH2O) or just above the max pressure to prevent wild running high.
Complex or Mixed Apnea (OA / CA)
The best CPAP therapy tends to be a low fixed pressure with no exhale pressure relief. Complex or Mixed Apnea is typically a mix between Obstructive and Central Apneas. For high levels of events Machine of choice is an ASV machine. These are among the most expensive of all PAP machines. Please post on the forums if you see this in your data. If an Auto band is used it is typically a very tight band.
What a person with complex sleep apnea needs is a machine that ONLY supports respiration during a central or hypopnea event. At all other times, spontaneous breathing should be supported and encouraged. What the ST does is provide the work of respiration at all times, and is intended for individuals who have obstructive pulmonary disease, or who need pressure support as a component of EVERY breath. ASV is the solution for central and complex apnea. ST and AVAPS is the solution for individuals with constant respiratory support needs.
Here is the approval criteria under Medicare (and most other insurance policies) for a bipap with backup rate; aka ASV. The device has a HCPCS Code of E0471 and includes a family of machines including ST and ASV. You definitely want ASV (adaptive servo ventilator) rather than ST (spontaneous/timed), which is an older technology. These devices are relatively expensive, and there are many forum members that have been through the process of getting ASV, and several that are actively going through it now. Anyway, insurance is going to require a polysomongraphy study that documents his central apnea. It may only show up when challenged with CPAP pressure, so you need to discuss with the doctor a referral for diagnostics to evaluate why you do not tolerate CPAP. The data and charts will let him see the severity of the problem. You must understand how the medical system and insurance reimbursement works to have a chance at advocating for this therapy. Here are a few links to get started.
- http://www.apneaboard.com/CSA-and-ASV-Updated-Morgan.pdf
- http://www.resmed.com/us/dam/documents/articles/1013495_Reimbursement_FF_RADs.pdf
- https://www.bcbsnc.com/assets/services/public/pdfs/medicalpolicy/noninvasive_respiratory_assist_devices.pdf
- https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/PAP_DocCvg_Factsheet_ICN905064.pdf
Central Apnea (CA)
Central sleep apnea (CSA) is a disorder in which your breathing repeatedly stops and starts during sleep. Central sleep apnea occurs because your brain doesn't send proper signals to the muscles that control your breathing. Central Apnea is best treated with an ASV machine. These are among the most expensive of all PAP machines. On an xPAP the best we can do is to minimize the Max pressure and utilize EPR or other relief (PS on BiLevel / BiPAP)if available, at the same time as raising the EPAP (min Pressure) to support obstructive events. These two treatments “fight” each other and it is a real balancing act. If an Auto band is used it is typically a very tight band.
The below is from RobySue from a forum post with minor edits by bonjour
When a PAPer is reporting problems with centrals while on xPAP, the important questions come down to these:
1) Did the sleep diagnostic test (the one without xPAP) show any centrals?
2) How many centrals are we talking about and at what pressure(s) do they start?
3) Can the OSA stuff (the OAs, the Hs, and most of the snoring) properly be treated at a pressure level that is below that needed to trigger the CAs?
4) Does the number of CAs go up, down, or stay about the same after a few weeks on xPAP therapy?
Here's the thing you need to be aware of: Some people's bodies do have a bit of a problem regulating the CO2 levels in the blood when they are first put on xPAP therapy for obstructive sleep apnea. And the result of not properly regulating the CO2 level in the blood leads to the emergence of central apneas. Essentially, you only inhale when the CO2 level in the blood is high enough for your brain to tell the lungs and diaphragm, "Inhale Now". When the brain misinterprets the CO2 level or if the CPAP washes out too much CO2, the brain doesn't send the signal to "Inhale Now" and you don't take a breath when you are supposed to take one.
The problem with pressure-induced centrals seems to be aggravated by the addition of pressure. In other words, the higher the pressure setting on the xPAP machine, the more likely pressure-induced centrals are to occur. In some people, the CAs can be completely controlled simply by limiting the max pressure the machine is allowed to use. Pressures over 10 cm are more likely to cause problems with CAs, and hence if the OSA stuff is controlled with a pressure less than 10, the usual fix is to just use only enough pressure to control the OSA stuff. (A few people have trouble with pressure-induced centrals at lower pressures; other people find that their pressure-induced centrals might only be a problem if the pressure is really high--like above 15cm.)
Sometimes the problem with pressure induced centrals is self-limiting: The body takes a while to figure out the whole xPAP thing, but after a few weeks it *does* adapt and by that point many people who had some issues with pressure-induced CAs notice that the number (and length) of the CAs in their data starts to decrease. And after a few more weeks of using their machine, the CAs essentially disappear---in other words, the person gets some isolated ones here and there, but the number of them is small and the overall AHI is consistently less than 5 (and often significantly less than 5) and the person reports feeling and functioning better in the daytime. The fact that many people's bodies take a while to adjust and that the number of CAs recorded often goes down with continuing to use the machine is a major part of why many sleep docs and most insurance companies don't just immediately switch an xPAP newbie from a CPAP/APAP or BiPAP/VPAP to an ASV machine at the first sign of pressure-induced centrals. Other reasons for not immediately switching include the cost of an ASV and the fact that learning how to sleep with an ASV can be much harder than learning how to sleep with a CPAP/APAP or BiPAP/VPAP due to the drastic pressure increases used to "trigger" inhalations as a way to prevent the central apneas.
Given that you are seeing some centrals and your overall AHI is sometimes in the 5-10 range instead of the 0-5 range, it's worth watching the centrals, but it is also worth giving your body some time to adjust to the AirCurve. And if you jumped from the AirSense to the AirCurve right away because of the centrals, then it really may be best to be patient for 2-4 more weeks of using the AirCurve with your current settings.
It's also worth mentioning that some people find that frequent changes to the therapeutic settings aggravates their problems with centrals. In this case, two important questions to ask are:
A) How long have you been using xPAP? (In this case, that means both the time you used the AirSense and the time you've used the AirCurve.)
B) How frequently do you change the settings? What is the longest you've used a particular setting?
EPR
EPR is exhale pressure relief. EPR acts a lot like pressure support (PS) with a bilevel (BiPAP/VPAP). To really understand its impact on therapy, you need to understand bilevel titration, where EPAP is used to resolve obstructive apnea, and pressure support (IPAP) can be used to manage flow limitation, hypopnea and RERA. A concern with EPR is that for patients with a CPAP titration based on fixed pressure, it actually can undermine the prescription, unless the CPAP pressure (IPAP) is increased.
For example, let's say you are titrated at 8 cm H2O pressure for CPAP. You get your new Resmed machine and dial in EPR at 3, and now instead of fixed pressure at 8.0, you now have bilevel pressure at 8/5. Well 5.0 cm EPAP pressure allows obstructive apnea to occur, so you find out you need a pressure of 11/8 and so you wonder why the clinic got it wrong. Happens all the time.
Compared to CFlex and AFlex used by Respironics, EPR is a true bilevel variable that is allowed as a "comfort feature". Flex is only a temporary pressure reduction at the beginning of exhale or inhale and is actually a comfort feature, and pressure returns to the CPAP level before exhale begins; but EPR acts like pressure support on a bilevel, and keeps the pressure low until inhale begins, unless the airway collapses and then the pressure stays low until the apnea ends.
This is all more than you wanted to know, but the point is bilevel therapy is much more comfortable than CPAP, and if you use EPR, it helps to understand how it might affect therapy.
- Start with a single CPAP pressure without EPR, for example 10 cmH2O
- Set EPR to 1 cmH2O AND increase CPAP pressure by the same amount as the EPR, so CPAP pressure is set to 10 + 1 or 11 cmH2O to continue the same support of Obstructive Apnea. This provides a range of 10-11 cmH2O on every single breath.
- Make small changes and evaluate.
It's important to understand how EPR works on a Resmed Autoset, and the difference between an Autoset and a bilevel machine.
On a bilevel, EPAP (exhalation positive airway pressure) is the pressure the machine provides when you're exhaling. This is what splints your airway against collapse. As you breathe in, the machine adds additional pressure, called pressure support (PS) to achieve IPAP (inhalation PAP). Note that PS is added to EPAP to achieve IPAP.
These terms are not really applicable to CPAP or APAP. The machine provides a pressure, which is just called "pressure". If you have EPR set, when the machine detects that you're starting to exhale, it reduces pressure by the amount of EPR. It is actually the reverse of pressure support on a bilevel machine. As the name suggests - exhalation pressure relief - EPR lowers the pressure. This is equivalent to lowering your EPAP (exhalation positive airway pressure). So if you need a certain EPAP to overcome obstructive events, increasing EPR will actually lower the EPAP below the required level and your obstructives - and obstructive hypopneas - will go up. (EPR does not "fight" hypopneas).
Other Software
MyAir (ResMed) Two values have more importance than the others, The AHI and the leak. The AHI is measure of the overall effectiveness of the treatment. The Leak as an indication that you need to look at more detailed information (OSCAR) to see if leak is really a problem.
- Usage Hours – Compliance Hours 10 points per hour, max of 70 points
- Mask Seal – 20 points for minimal mask leak, 10 to 15 points for moderate leak, and 0 to 10 points for higher leak. Mask type dependent.
- AHI / Events per hour –minimal events, you get 4 to 5 points
- Mask on/off –Every mask removal greater than one loses a point. If you get up to relieve yourself that is a point down.
- 14 day snapshot
The overall scoring is good for encouraging compliance. For me non-compliance is a night without any sleep or with minimal sleep. I ALWAYS use my xPAP, there is no question of compliance with me.
DreamMapper (Philips)
- Usage
- AHI
- Mask Fit
- Up to 90 day views
Tips and Tricks
- Leak Rate Chart -- With OSCAR look at your Leak Rate graph where it is shaded (large leak/ LL), flat tops on this graph suggest mouth breathing.
- ResMed in OSCAR right click on the left header of the Leak Rate graph and click on Dotted Lines then select "Leak Rate Upper Threshold" to get a line across the graph.
- Respironics the value varies and is considerably larger than for ResMed because leaks are measured differently. Conservatively you can use a leak rate 60 but you have to set this manually.
- Severity depends on how much over this threshold and for how long it is in the Large Leak territory.
- Flow Rate Chart
- in OSCAR right click on the left header of the Flow Rate graph and click on Dotted Lines then select "Zero" to get a line across the graph that divides Inhalation and Exhalation.
One clue on CA vs OA is the flow around the event. When breathing ends on an inhale, it is almost always a SWJ (Sleep Wake Junk) change in position or CA. Most CA events terminate with normal breathing restarting, not a strong recovery breath(s). Events beginning in a flow limitation (down-sloped peak inspiration) and especially when followed by recovery breathing are clearly OA. It's not possible to accurately know what a CPAP flagged event 'really' is, but you can second-guess them pretty well.
Here are the AHI levels of severity for Sleep Apnea in adults:
Mild: 5-14
Moderate 15-29
Severe: 30+
Here are the AHI levels of severity for Sleep Apnea in children:
Mild: 1-5
Moderate 5-10
Severe: 10-30
Extremely Severe: 30+
What Not To Do
CPAP dial winging... Not establishing a treatment routine and changing the numbers without a plan, with no idea why you're doing it, or what it might accomplish...good luck with that.
- Success at xPAP is a process that takes some time, consistency, trial and error and learning. Choose a thread where you want to post your experiences and data, and stick with it. That way we all see what is working, or not, and have the history in one place.
- Develop a treatment plan and stick with it. We are in this for the long haul. It takes time to observe results and decide on the next step. If you make changes to your settings, understand what those setting changes can do, and cannot do. Even small changes can make a difference for better or worse. As you get closer to your treatment goals smaller changes and longer times between changes will lead to success.
Principiles and Terms of Titration
Hardware:
In order for an Autotitrating PAP to measure breathing patterns properly and detect abnormal events, flow and pressure must be communicated to the algorithm as a high-quality signal. The principle behind the use of pneumotachometers and flow sensors is that flow patterns indicate corresponding breathing patterns. Autotitrating PAPs also use a pressure transducer to deliver precise pressure levels.
Responding Events:
Breathing events that, when present, trigger a response to increase pressure and, when absent, trigger a response to decrease pressure.
Obstructive Apneas – occur when patient airways close and breathing cannot occur
Hypopneas – occur when patient airways are partially closed and breathing is limited
Predictive Events:
Snoring and Flow Limitation are similar in that both may occur prior to obstructive apneas and/or hypopneas. All Autotitrating PAPs are proactively programmed to increase pressure in response to snores or flow limitations to prevent the occurrence of obstructive apneas and hypopneas. There is conflicting evidence as to which parameter allows the earliest response.
Non-Responding Events:
Breathing events that are identified and logged without triggering a pressure response. Most Autotitrating devices have two non-responding events in common:
Leaks – usually caused by mouth breathing or mask fit/seal leaks
Non-obstructive apneas including Central Apnea and Clear Airway events – may occur during OSA therapy if the PAP pressure reduces the normal carbon dioxide accumulation and degrades the CO2 stimulus response. May also be primary Central Apneas that cannot be properly defined by an Autotitrating device alone.
NOTE: Non-obstructive apneas in excess of 10 per hour could indicate primary central apneas and clinical intervention may be required.
DISCLAIMER & LEGAL NOTICE
BY USING OUR CPAP SETUP DIRECTIONS, SETUP GUIDES AND PRESSURE-CHANGING RECOMMENDATIONS, YOU UNDERSTAND THAT YOU ARE PERSONALLY ASSUMING ALL RISK FOR USING INFORMATION ON THIS WEB PAGE AND IN THESE DOCUMENTS AND WILL NOT HOLD APNEA BOARD, ITS MEMBERS, OWNERS, ADMINISTRATORS AND MODERATORS LIABLE FOR ANY PROBLEMS, DAMAGES, PHYSICAL HARM, (INCLUDING DEATH), MENTAL HARM OR ANY OTHER HARM THAT MAY COME TO YOU, YOUR FAMILY MEMBERS, FRIENDS, CO-WORKERS OR ANY OTHER PERSONS WHO MAY RECEIVE THIS INFORMATION FROM YOU. YOU MAY NOT USE, COPY OR DOWNLOAD THESE DOCUMENTS UNLESS YOU HAVE A LEGAL RIGHT TO DO SO UNDER ALL APPLICABLE U.S. LAWS. INFORMATION CONTAINED ON THIS WEB PAGE, APNEA BOARD FORUMS AND ON THE APNEABOARD.COM WEB SITE SHOULD NOT BE CONSIDERED AS MEDICAL ADVICE. ALWAYS SEEK THE ADVICE OF A QUALIFIED PHYSICIAN BEFORE SEEKING TREATMENT FOR ANY MEDICAL CONDITION, INCLUDING SLEEP APNEA. ALWAYS SEEK THE ADVICE OF A QUALIFIED PHYSICIAN BEFORE CHANGING PRESSURE ON ANY MEDICAL DEVICE, INCLUDING CPAP MACHINES.

Donate to Apnea Board