Beyond AHI: Apneas and hypopneas in the Flow Rate graph
Contents
Introduction
- This article is part of the CPAP_Data_Interpretation series.
- See also OSCAR_Help.
- Acknowledgement: Much of the material in this help system has been taken and/or adapted from RobySue's Beginner's Guide to SleepyHead
Most sleep doctors and most OSA patients never really concern themselves with detailed efficacy data beyond the nightly and long term AHI data. And that's ok: If the nightly AHIs are always below 5.0 and you're feeling well, there's really no need to look at the detailed data available in Oscar about each and every event the machine recorded over night. But if you're a data hound, the stuff you can see in the Flow Rate data can be fascinating. And if you're not feeling as well as you hoped with CPAP therapy, sometimes examining the Flow Rate data in more detail can shed some insight into what might be going on.
The information on this page is written for the curious CPAP users who simply wants to know more about what the Flow Rate data shows and what it may indicate about the quality of therapy. None of this information should be considered medical advice. If you are experiencing problems with your CPAP therapy, you should consult your sleep doctor.
Flow Rate graph: A trace of every breath you took
When we use a CPAP, our upper airway is part of a "semi-closed pressurized system" comprising the blower, the tube, the mask, and our upper airway. The system is "semi-closed" because of the intentional leakage built into the mask to prevent re-breathing. A full efficacy data CPAP measures the back pressure at blower end of "system" and uses that data to calculate the air flowing into and out of our lungs all night long. The resulting data is called the Flow Rate data, and the Flow Rate graph provides a trace of very breath you took all night long.
To understand how to read a Flow Rate graph, it helps to zoom in to the point where the individual breaths can be seen:

The y-values are measured in Liters per minute (L/min). When the Flow Rate is positive (above the horizontal line labeled as 0.0), the air flow is going into the lungs and you are inhaling. When the Flow Rate is negative (below the horizontal line labelled as 0.0), the air flow is going out of the lungs and you are exhaling. The farther away from the 0.0 line, the more rapidly the air is moving. So a large positive bump represents a strong, deep inhalation, whereas a large negative bump represents a strong, deep exhalation. The transition between inhalations and exhalations occurs when the Flow Rate graph crosses the 0.0 line. Pauses in breathing show up as flat spots in the Flow Rate at the 0.0 line.
Normal sleep breathing, such as shown in the above graph, is very regular in the size and shape of the inhalations and exhalations. Normal sleep breathing is usually much more regular than normal wake breathing, and typically the size of the inhalations and exhalations is smaller in sleep breathing than in wake breathing.
Basic scoring criteria for apneas and hypopneas
Each event that is scored by your machine shows up as a tick mark in the Flow Rate graph if this facility is turned on (see Common features of detailed graphs). Zooming in on the Flow Rate curve often shows exactly why the event was scored; but sometimes it is not clear why an event was (or was not) scored. And since our CPAPs do not have EEG data, they cannot tell when we are awake and when we are asleep. Hence your CPAP will score "events" that meet the definitions in their scoring algorithm even if you are wide awake.
Each machine's manufacturer has its own algorithms for scoring (and classifying) apneas and hypopneas. These algorithms are not perfect-- we'll look at that later. But they are very good.
Rather than looking at each individual CPAP maker's definitions of apnea and hypopnea, we'll generalize the basic concepts that underlay all their algorithms
- Moving Baseline Flow Rate. All full efficacy CPAPs compute a moving baseline flow rate using several minutes worth of data. The typical time frame is a five minute window of some type: The machine looks at all the breaths in the last five minutes and uses that information to compute an average or baseline flow rate. (The particulars of how this baseline is computed are NOT the same on all CPAPs, but those particulars don't change a basic understanding of how events are scored.) It's enough for now to think of the moving baseline flow rate as the "average" size of your inhalations for the last five minutes or so. Apneas and hypopneas are scored when there is a measurable and significant decrease in the Flow Rate as compared to the moving base line average and that decrease lasts for at least 10 seconds.
- Apneas. Typically an apnea is scored when the Flow Rate is reduced by at least 90% from the moving baseline average for at least 10 seconds. In other words, during a machine scored apnea, the air flow into (and out of) the lungs is less than 10% of the moving baseline airflow. This is enough of a reduction in airflow that the Flow Rate curve typically looks pretty flat and it's clear that little or no air is moving into or out of the lungs.
- Hypopneas. Typically an hypopnea is scored when the Flow Rate is reduced by at least 50% from the moving baseline average for at least 10 seconds. In other words, during a machine scored hypopnea, the air flow into (and out of) the lungs is less than 50% of the moving baseline airflow. The actual amount of air flow reduction needed to score a hypopnea depends on the manufacturer. DeVilbiss allows the criteria for scoring a hypopnea to be customized: The reduction in airflow can be set anywhere between 30% and 70%.
It's important to remember that on an in-lab sleep test (PSG), you have to be asleep at the beginning of the event for it to be scored as a sleep disordered breathing event. And that means that EEG data must be used in scoring real sleep disordered events on a PSG. But our CPAPs do not have any EEG data to work with, and any time the Flow Rate meets the manufacturer's definition of an apnea or hypopnea, the machine will score the event. The working assumption is: If you have the mask on your nose, there's a high probability that you are asleep and the event is "real." Whether the assumption that you are most likely asleep, however, may not be a valid assumption in some circumstances. We'll return to this idea in a bit.
Obstructive and central apneas
On an in-lab sleep test (PSG), each apnea will be classified as either an obstructive apnea or central apnea. The data from the belts around the chest and abdomen are used to distinguish between the two types of apnea on a PSG. If the belts indicate that the patient is trying to breathe, but no air is getting into the lungs, then it's assumed that the problem is that the upper airway has collapsed and the apnea is scored as an obstructive apnea. But if the belts indicate that the patient is making no effort to breathe, then it's assumed that the problem is that the brain has "forgotten" to send the signal to the diaphragm and lungs to inhale. The patency of the airway is irrelevant when scoring a central apnea on a PSG because the main problem is with the brain's forgetting to tell the diaphragm and lungs to breath. And it's possible for the airway to collapse during a central apnea.
But our CPAPs have no way to determine the effort to breathe. Hence CPAPs cannot distinguish between obstructive and central apneas in the same way that the technician monitoring a PSG does. Originally full efficacy data CPAPs did not try to distinguish between obstructive and central apneas. (The Fisher & Paykel Icon still does not try to distinguish types of apneas.) But when manufacturers started designing Auto CPAPs, a potential problem had to be addressed in the Auto algorithms: A minority of CPAP users are sensitive enough to pressure to develop problems with pressure-induced central apneas. And the tendency to have problems with pressure-induced centrals is more pronounced the higher the pressure setting on the CPAP. Hence early APAP Auto algorithms often were designed to NOT increase the pressure in response to apneas scored at pressures of 10cm or greater. In an effort to get around this difficulty, many of the current generation of full efficacy CPAPs make an effort to distinguish between apneas are presumed to be obstructive and those that are presumed to have a high probability of being central, and an APAP with such a "central apnea detection" algorithm can be programmed to respond to the apneas classified as obstructive and ignore the other apneas.
ResMed and Philips Respironics CPAP machines use (different) proprietary algorithms to test the patency of the airway and use the result to classify each apnea as a clear airway apnea (CA) or an obstructive apnea (OA). When the data from the algorithm leads to an ambiguous result, the apnea may be scored as an unknown apnea (A or UA). Both ResMed and Philips Respironics Auto machines will increase the pressure in response to clusters of OAs, but they will not increase the pressure in response to apneas scored as CAs. (Note that ASV machine do in fact respond to central apneas).
DeVilbiss machines use a very different algorithm to classify each apnea as an apnea (A) or a non-responding apnea (M or NRA). A DeVilbiss Auto machine will increase the pressure in response to events classified as "apneas", but it will not increase the pressure in response to "non-responding" apneas.
As near as I can tell, Fisher & Paykel machines do not try to distinguish the type of apnea. And I have not been able to find any specific information about how the Fisher & Paykel Icon responds to machine scored apneas.
It's also important to remember that the ResMed and Philips Respironics algorithm for distinguishing between OAs and CAs and DeVilbiss algorithm for distinguishing between As and NRAs are not infallible. They are prone to misclassifying apneas under certain circumstances. For most users, it's not a huge problem, but for a small number of users, it can be an issue. We're not familiar enough with the DeVilbiss alogrithm to have a good sense of its limitations. But both the ResMed and Philips Respironics algorithms are based on using variations in the CPAP pressure to test the patency of the upper airway. As such they both have the same broad characteristics:
- A CA scored by either the ResMed or Philips Respironics CA algorithm is very likely to be a "real" CA in the sense that the airway is clear (open). As such, a real OA is not very likely to be mis-scored as a CA on either a ResMed or Philips Respironics machine.
- Scoring a real central apnea (as scored on an PSG) does not depend on the patency of the upper airway; hence there is a higher probability that a real CA may be mis-scored as an OA by the Philips Respironics and ResMed CA detection algorithms
- Both the Philips Respironics and ResMed CA-detection algorithms are more likely to have problems detecting CAs at higher pressures. In other words, as the pressure increases, the chances that a CA is mis-scored as an OA increase
Other flagged events
In addition to scoring apneas and hypopneas, many CPAP machines score snoring and/or flow limitations (FL). The way machines score this things varies quite a bit, and they are discussed at length in 10. Snoring Data and 11. Flow Limitations.
In addition to scoring OAs, CAs, Hs, snoring, and FLs, the Philips Respironics System One machines also score respiratory effort related arousals (RERAs) and periodic breathing (PB) in the events table with flags on the Flow Rate curve.
RERAs
On an overnight PSG, a RERA is scored when there is evidence of increasing respiratory effort that ends with an EEG arousal. Not all labs score RERAs, by the way. The line between RERA and an AASM Rule 4B "hypopnea with arousal" is a bit arbitrary: RERAs don't have have last 10 seconds, but 4B hypopneas do; RERAs do not require a 50% reduction in airflow, but 4B hypopneas do. And a RERA requires an EEG arousal, whereas a Rule 4B hypopnea requires either an arousal OR an O2 desat of 3%. Finally a RERA may nor may not have an O2 desat. When a lab chooses to score RERAs, the lab will usually compute both an AHI and an RDI:
- AHI = (number of OAs + CAs + Hs scored)/(total sleep time)
- RDI = (number of OAs + CAs + Hs + RERAs scored)/total sleep time)
There are people whose PSG indicates that they a normal diagnostic AHI (less than 5), but who experience enough RERAs for the RDI to be seriously elevated. Such people often wind up with a diagnosis of upper airway resistance syndrom (UARS) instead of OAS. The connections and differences between UARS and OAS are still being debated in the sleep medicine community. But the usual treatment for UARS is CPAP therapy since CPAP can be used to smooth out the breathing and prevent the RERAs from happening.
Since a RERA requires an EEG arousal to be scored and there is NOT a clear definition of how much the flow rate must be reduced for a RERA to be scored, most CPAP machines do not attempt to flag RERAs. But Philips Respironics has developed a proprietary algorithm for scoring what it believes are RERAs. Since there is no EEG data, the Philips Respironics RERA algorithm is based on a statistical analysis of what the wave flow for real RERAs on PSGs looks like: Loosely, the Philips Respironics RERA algorithm looks for evidence of increasing respiratory effort (i.e. "flow limited breathing") followed by one or more "recovery" breaths. When we look at the RERAs scored in our sample patient's data, it's sometimes difficult or impossible to see both the "evidence for increasing respiratory effort" and the "recovery breaths". We've also noticed that the placement of the RERA tick mark is far less consistent: Sometimes it appears at the beginning of the RERA, sometimes it appears at the end, and sometimes it appears in the middle. But every now and then we see a RERA where it is easy to see why it was scored:

Because the RERA algorithm is proprietary and is based on just flow rate data rather than (flow rate + belts + EEG), it's important to understand that RERA flagging by the Philips Respironics machines should be considered an "extra" that is probably not always accurate. The RERA algorithm probably flags things that aren't real RERAs and it probably misses some real RERAs as well.
Nonetheless, if your sleep study showed a large number of RERAs the Philips Respironics RERA scoring algorithm may be useful for partially monitoring how well the CPAP is doing in terms of preventing RERAs from occurring.
Periodic Breathing
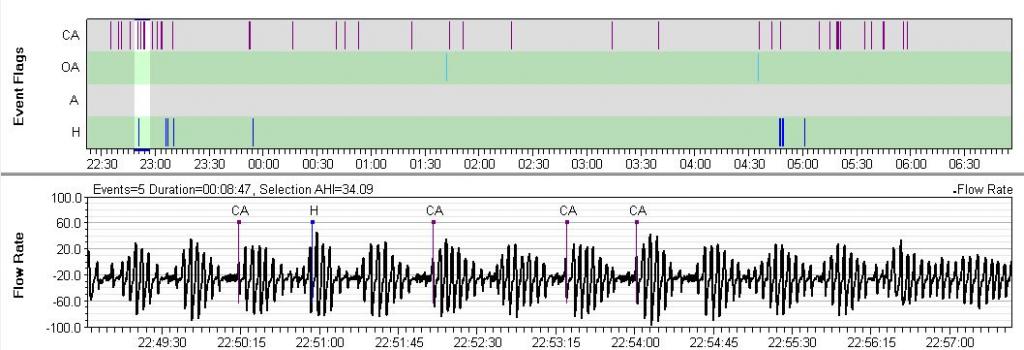
Philips Respironics machines flag breathing that meets their definition of periodic breathing (PB). On the Philips Respironics web pages PB is defined as, "Periodic breathing is defined as alternating periods of hyperventilation with waxing/waning tidal volume..." Typically the waxing and waning pattern must be quite regular in visual appearance and it must present for at least a minute or two for PB to be scored. PB is flagged with a green back ground on the flow rate data. Often, but not always, there will be CAs (or Hs or sometimes OAs) scored at the nadir of the cycle. Sometimes the System One will only flag the most obvious part of the cycle:

A bit of PB now and then is nothing to worry about. However, there is one form of PB that is called Cheyne-Stokes Respiration (CSR) that is clearly associated with some forms of heart disease, including congestive heart failure. CSR is very regular and has a CA at the nadir of the cycle (although the CA may be mis-scored as an OA). If you have serious heart disease and you see a lot of PB scored in your flow rate data, it is worth mentioning it to your cardiologist as well as your sleep doctor.
Detecting Periodic Breathing on other CPAPs
Once you know what PB looks like, you can often spot suspicious patterns by simply scrolling through the Flow Rate data in with a 5-10 minute window. Any periodic waxing/waning patterns will be show up at that magnitude. Whether this is worth doing on a regular basis is another question altogether. Unless you have a co-morbid condition that is associated with PB (such as congestive heart failure), PB is not something you need to spend much time worrying about or trying to locate in your data.
Here's an example of PB that may be CSR pulled from a ResMed machine:
Sleep / wake breathing and "false" events
Wake breathing
Because the scoring of an apnea or a hypopnea depends on the moving baseline airflow, the actual airflow recorded during an apnea or a hypopnea can vary. This becomes important during periods when you are not soundly asleep. Wake breathing is controlled by the voluntary nervous system and it is much more variable than sleep breathing. Because of this variability it is not uncommon for OAs, CAs, and Hs to be scored during periods when you are awake: A few minutes of conscious deep yoga style breaths followed by a return to normal wake respiration may meet the criteria to be scored as an H. When we're tossing and turning in bed, it's not uncommon to hold our breath for a few seconds while concentrating on turning over or fixing the bed pillows and covers; if the pause in our breathing is close to 10 seconds, it can be mis-scored as a hypopnea. And some people's wake breathing patterns are more susceptible to being misinterpreted as sleep disordered breathing than others. These sleep/wake/junk dozing periods are most likely to happen at the beginning or end of the night, particularly if you are in the habit of lying in bed without being sound asleep.
Sometimes patients will lie in bed trying to get back to sleep if they're not quite ready to get up; sometimes they can be restless before admitting that they're not likely to get back to sleep. If you're like this and look at your data after one of these mornings, you may see a lot of sleep/wake/junk breathing. Here's a close up of what sometimes happened when our sample patient lied in bed unsuccessfully trying to get back to sleep:

In this data, it's clear that the patient never got soundly back to sleep not only because of the large number of (false) events, but also because she turned the BiPAP off and back on three additional times after the first wake around 8:10 before finally deciding to crawl out of bed at 9:00. During this wakeful period, 4 Hs, 1 CA, 2 OAs, 3 FLs, 1 RERA, and some snoring were all scored. All of them are likely artifacts of her wake breathing and/or irregularities in her breathing scored as she was just starting to doze before waking back up. On a PSG, most or all of these events would probably not be scored based on EEG data-- an event has to start in SLEEP in order to be scored as sleep disordered breathing.
Distinguishing this kind of sleep/wake/junk (SWJ) breathing from periods of seriously sleep disturbed breathing periods that indicate your CPAP therapy may not be optimized is not particularly easy. But extremely restless looking periods at the beginning or end of the night are more likely to be SWJ. And if you know you were awake for long periods of time during the night, clusters of events during the times you were awake (or restless) are likely to be SWJ.
Sleep transition breathing
Sleep transition breathing also poses problems for our machines. The control of respiration has to be handed off from the voluntary nervous system to the autonomous nervous system. it is not uncommon that during the transition process, the airflow into the lungs drops (and a breath or two is skipped) as the body resets the CO2 trigger for inhalation. On a PSG, these "sleep transitional central apneas" are not scored because they are not part of sleep disordered breathing. But our machines cannot tell that we're in the process of transitioning to sleep, and it's not uncommon for "false" events to be scored just as we're drifting off to sleep.
Here is an example of a sleep transition central apnea from our sample patient's data:

Contrast the above sleep transitional central apnea with what appears to be a real central apnea:

Lengths of individual events
SleepyHead has a neat tool that both lets you zoom in on a particular event and (estimate) how long it lasted. Between the Calendar and the AHI table in the standard view of the Daily Data table there is a navigation menu that looks like this:
Clicking on the Events tab changes the look of the Left Side Bar; once Events is selected, the Left Side bar looks like this:

You will notice this is a list of the kinds of events that were recorded for the night. Clicking on the little triangles by each event type brings up a list of the the individual events of that type:

For CAs, Hs, and OAs on an S9, the number in parenthesis beside the event is the length of the event measured in seconds. On other machines, those numbers are event markers of some sort and they may or may not provide a reasonable estimate of the length of time (in seconds) of the event.
- ResMed: The numbers in parenthesis are the length of the event measured in seconds.
- Philips Respironics System One: The numbers are event markers. For CAs, OAs, Hs, PBs, and LLs, the numbers are usually a good approximation of the event length measured in seconds. For RERAs, it appears that the number is a good approximation of the event measured in seconds. For VS, VS2, and FL it is not at all clear what the meaning of the numbers is. SleepyHead uses the VS2 numbers to draw the Snore graph; presumably the higher the number attached to a VS2, the louder OR longer the snoring. It's not clear which. For more information on how the Philips Respironics scores snoring see 10. Snoring Data.
- DeVilbiss IntelliPAP: The numbers in the parenthesis are usually single digit numbers and it is not clear what their meaning is. Since the IntelliPAP does not record Flow Rate data, it is impossible to see whether there is some connection between these numbers and the lengths of the events.
- Fisher & Paykel Icon: The numbers in parenthesis seem to always be 1, and hence they are not related to the length of the event. You can zoom in on each event in the Flow Rate curve and estimate the length of the event visually.
Clicking on a particular event in the Events list immediately zooms all the Daily graphs into a close up view of the chosen event. The time frame for the event is controlled by the number on the slider bar at the end of the Events list: The smaller the number, the closer we zoom in:
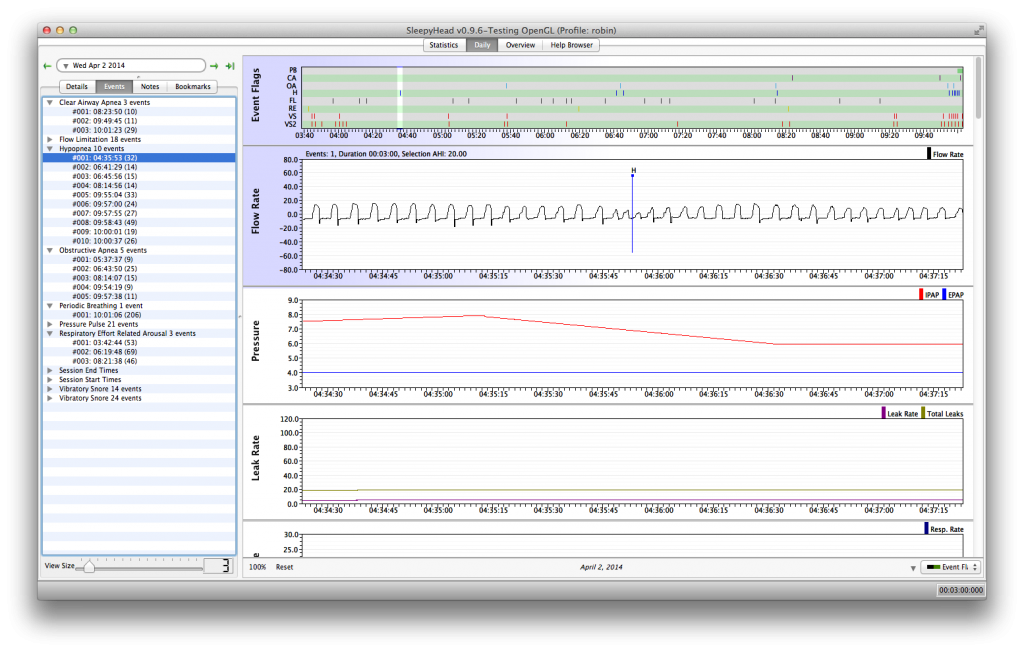
This particular hypopnea's flag is more or less in the middle of the hypopnea. Most of the time the flag is closer to the end of the event, but there is some variability. Another thing that's worth pointing out is that the patient's BiPAP is in the middle of decreasing the IPAP as part of the Philips Respironics "search" algorithm; the isolated H does not cause the machine to increase the IPAP and that's a bit counter intuitive to some CPAP users. But it is how the Philips Respironics Auto algorithm works: It ignores isolated Hs and OAs; pressure is increased for events only if two or more events occur very close to each other.
Clusters of events
One common concern CPAP users have about their data are clusters of events. It's important to understand that your CPAP machine is not going to prevent every apnea. If you have a bad night now and then with some clusters of events, it's not something to worry too much about. But if you tend to see dense clusters of events on most nights, your CPAP therapy may not be optimized.
Figuring out what's causing clusters of events can be difficult: Sometimes clusters of events occur in REM sleep. Sometimes clusters appear during back sleeping. Sometimes clusters of events are just sleep/wake/junk breathing. Occasionally clusters of events may be an indication that you're in the unlucky 10-15% of CPAP users who have problems with pressure-induced central apneas.
There's no clear way to tell what caused any particular cluster of events. Our CPAPs do not have EEGs and there's no way to definitively tell when REM sleep is occurring in the data. Likewise our CPAPs have no position detector, so the data can't directly tell us whether supine sleep is the problem. If you remember being awake or restless at certain period in the night, then it may be possible to identify a cluster as probably being sleep/wake/junk, but it's not uncommon to have no real memories of a restless period during the middle of the night. Long clusters of central apneas at times you think you were asleep obviously raise the question about pressure induced centrals.
If your diagnostic sleep study indicated that your OSA is much worse in REM and the clusters are roughly 90 minutes apart with longer clusters towards the end of the night, they may very well be REM related. If your diagnostic sleep study indicated that your OSA is much worse in supine sleep and you find yourself waking up on your back at times, then the clusters may be supine-sleep related. But there really is no way to tell for sure that clusters of events in your data are REM or supine sleep related. Sometimes its worth making the reasonable assumption that the clusters are REM or supine sleep related in these situations, and if the clusters are particularly persistent (as in they occur on most nights) and nasty (as in they involve a lot of events), it's worth checking with your sleep doctor since a (small) increase in pressure may help break up the clusters. But if the clusters continue after one or more pressure increases, more formal investigation into their cause may be needed.
How APAP machines respond to events
New CPAP users are sometimes surprised by the fact that their CPAP did nothing when an apnea was in progress. There's an assumption that the positive air pressure provided by the CPAP is supposed to "blast" through the obstruction and restart the breathing. But pressure is not used to try to "end" an on-going event. It's not even clear that 20cmH20, the maximum pressure delivered by a CPAP, would even be effective at trying to "blow" a collapsed airway open: 20cmH20 is not enough pressure to effectively blow up an ordinary balloon. In fact, 20 cmH20 is about the difference in atmospheric pressure between a very stormy, low pressure day, and a bright sunny high pressure day.
The basic idea in CPAP therapy is to provide (a small bit of) positive air pressure through the entire breath cycle to make it more difficult for your airway to collapse. This system is very good at preventing apneas and hypopneas from occurring, but it is not perfect: A few events will likely occur each night, but the overall number of events will be low enough to keep your treated AHI under 5.0, and probably well under 5.0, each night you use the machine. In other words, a well-adjusted CPAP makes it difficult, but not impossible for your airway to collapse.
CPAPs, of course, cannot respond to OAs and Hs by increasing pressure since they have one fixed pressure setting. APAPs do respond to OAs and Hs, but it's important to realize that an APAP will wait until the apnea or hypopnea is over before it increases the pressure. And even then, a typical APAP won't raise the pressure after each and every OA or H. Rather, APAPs will only raise the pressure in response to OAs and Hs if two or more events occur in a relatively small amount of time like 5 minutes or so. The rationale for this behavior is based on the AASM Clinical Guidelines for Manual Titration Sleep Studies. Isolated OAs and Hs are not necessarily indicative of a badly compromised airway: Even normal people have the occasional (frank) OA or H during their sleep. But two or more OAs or Hs occurring close together indicates that the current pressure may not be sufficient to prevent the airway from collapsing in the (very near) future. And since more pressure is needed to prevent future events from happening, the machine increases the pressure after the second (or latest) event in the cluster ends.
APAPs also respond to snoring and flow limitations by increasing the pressure. Snoring and flow limitations are considered precursor events to OAs and Hs. In other words, snoring and flow limitations are thought to indicate that the airway is compromised: It may be partially collapsed (but not far enough to score an H) or it may be just barely beginning to collapse. More pressure at this point will help hold the airway open and prevent further collapse, and hence, prevent OAs and Hs from occurring. It's worth noting that some brands of APAPs are very aggressive in how fast and how far they increase pressure in response to snoring or flow limitations.
So the overall goal in every manufacturer's Auto-algorithm is to increase the pressure just enough to prevent more events from happening in next few minutes and allow the breathing to stabilize. The idea is to avoid jacking up the pressure unnecessarily: That can lead to more unstable breathing, discomfort, and more pressure than is needed to keep the airway open most of the time. And once the machine is satisfied the breathing is indeed stable, the Auto-algorithm will decrease the pressure until there is evidence that the airway is once again in some danger of collapsing.
Each manufacturer's Auto-algorithm handles the details of how to handle the pressure increases and decreases in its own proprietary way. Some machines are more aggressive and increase pressure faster in response to snoring, flow limitations, and events. Some take small 1cm steps in increasing the pressure and then wait for a minute or more before increasing the pressure further. The Philips Respironics machines even have a search algorithm that periodically tests what happens to the Flow Rate curve when a modest pressure increase is applied even when there are no scoreable events (OAs, Hs, FLs, RERAs, and Snoring). And likewise, each manufacturer's algorithm has a different way of deciding when to start decreasing the pressure and how fast to decrease the pressure.
It's clear from reading informational material aimed at clinicians, that each manufacturer believes that they have the "best" algorithm. But what little information that has been published about independent bench trials seems to indicate that while real differences in the auto-algorithms can be quantified, the clinical significance of those differences is much harder to evaluate. This may be one reason that some sleep docs are so reluctant to prescribe APAP therapy as the first course of treatment for ordinary OSA.

Donate to Apnea Board