Flow limitation
Flow limitation may be inspiratory (during inhale) or expiratory (during exhale). It refers to any condition which impares the flow-rate of air through the respiratory tract. Inspiratory Flow limitations occur to many individuals that are diagnosed with obstructive sleep apnea. Inspiratory Flow Limitation (IFL) is an increasing resistance in inspiratory flow that slows the volume and flow of air as the inhale proceeds. It is visualized in a flow rate graph as a flattened or downward sloping wave-form rather than a smooth peak. Expiratory Flow Limitation (EFL) is similarly restricted flow rate during the exhale cycle. Flow limitations can result from anatomical narrowing of the airway, airway obstruction, and positional obstruction where the airway is restricted due to an individual's sleep position resulting in occlusion of the airway. EFL may also result from an intolerance to CPAP pressure during exhale. Both IFL and EFL seem to respond well to bilevel therapy where the exhale positive air pressure (EPAP) is a lower pressure than the inhale positive air pressure (IPAP).
Related articles Flow Limitation/UARS and BiPAP a physician's perspective by Barry Krakow MD. Oscar Flow Limitations Oscar User's Guide to Flow Limitation.
Contents
Flow limitations
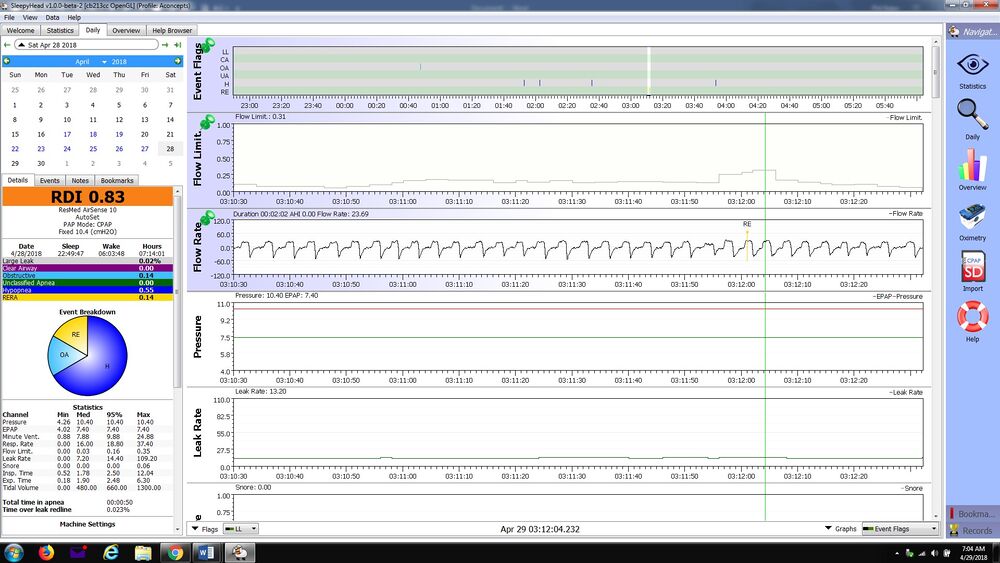
The images below are an example of a forum member that was experiencing severe flow limitation. The complaints were that the Resmed Airsense 10 Autoset CPAP which was originally set to a minimum pressure of 6 and maximum pressure of 16, was reaching uncomfortably high pressures, remaining near the maximum pressure most of the night. The user experienced discomfort and a high incidence of respiratory event related arousals (RERA). A high rate of flow limitations was causing pressure to increase without corresponding therapeutic benefits. It was recommended that the user reduce the maximum pressure to 11.0 cm, and increase exhale pressure relief (EPR) to 3. In bilevel terms, this was equivalent to increasing pressure support (the difference between IPAP and EPAP). If this was a bilevel, pressure settings would be expressed as EPAP 6.0 to 8.0 with pressure support of 3.0 cm. The images show the progress experienced by increasing the EPR level from a setting of 1 to a setting of 3. The first image is a very good example of "typical" inspiratory flow limitations.
How Philips Respironics and Resmed Calculate Flow Limitation
In order to evaluate flow limitations, Respironics determines roundness, flatness, skewness, and WPF to rate the most recent four breaths as better, worse, or the same compared to baseline. Roundness is determined by the similarity of the WPF between 5% and 95% values to a sine wave. Flatness is determined by the absolute value of the variance between 20% and 80% of inspiratory flow from the average of all the values in the same period, divided by 80% volume point. Skewness is determined by dividing the average of the highest 5% of flows in the mid third of the breath by the average of the highest 5% of flows in the first third of the breath.
ResMed also determines flow limitation. S8 AutoSet defines flow limitation using flatness of an inspiratory breath. The flatness index is calculated by the RMS deviation from unit scaled flow calculated over the middle 50% of a normalized inspiratory breath. From the S9 onward, flow limitation is calculated using a combination of flatness index, breath shape index, ventilation change, and breath duty cycle. Ventilation change is the ratio of the current breath ventilation to recent 3-minute ventilation. Breath duty cycle is the ratio of current breath time of inspiration to total breath time of recent 5 minutes. If a breath is severely flow limited, the flow limitation index will be closer to one and when the breath is normal or round, the flow limitation index will be zero. [1]
Flow Limitation in Positional Obstructive Apnea
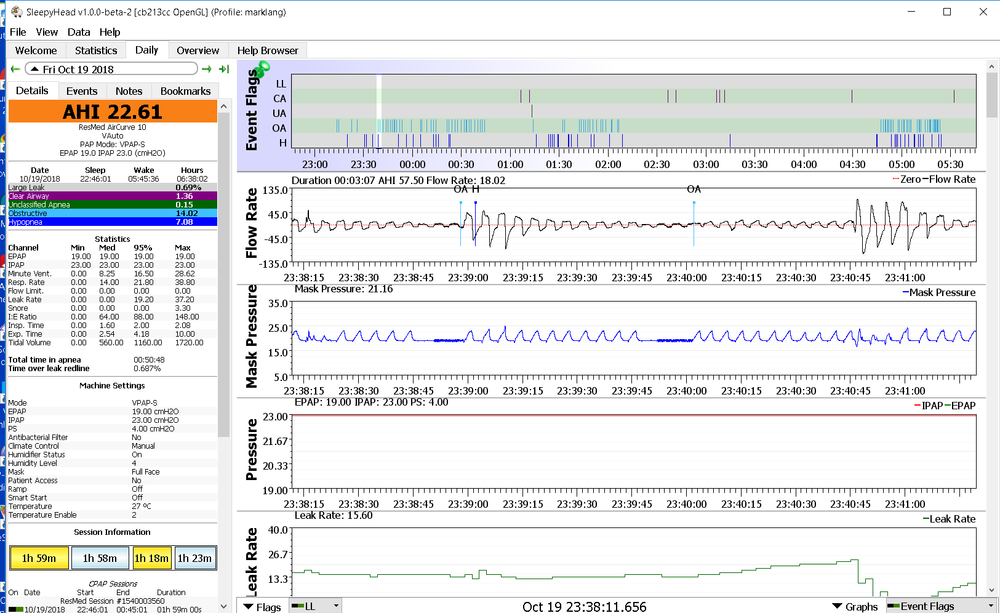
This forum thread shows an example of severe obstructive apnea with flow limitation. CPAP Produces Variable Results New User With help from forum members, it was recognized that the culprit for the numerous events was a positional apnea. The important clue was the flow limitations in the user's chart that showed severe restriction of flow. This can be seen on page three of the thread the following graph. The member Marklang was using a Popitz ergonomic pillow, and resolved the apnea and flow limitation with a combination of a soft cervical collar and a Resmed Aircurve 10 Vauto bilevel to achieve AHI less than 1.0.
Examples of respiratory wave form abnormalities including Flow Limitation
EPR and Pressure Support As Tools to Mitigate Flow Limitation
"Pressure Support" is the difference between inspiratory positive air pressure (IPAP) and expiratory positive air pressure (EPAP). EPR (expiratory pressure relief) is a form of bilevel pressure support used in Resmed CPAP machines, and in several other CPAP implementation. In the OSCAR mask pressure chart, it looks identical to the pressure delivered by the Aircurve Vauto, but limited to a maximum of 3-cm. Flow Limitation is most often "Inspiratory Flow Limitation", and pressure support (EPR) works by supporting or supplementing the spontaneous respiratory effort during inspiration. This overcomes the tendency of the airway to collapse during inspiration by providing proportionally higher pressure as a breath progresses to it's peak flow. Inspiration occurs because the chest expands creating negative pressure in the upper airway (vacuum), and this is the mechanism of flow limitation and obstructive apnea. Without pressure support, flow limitation in some individuals is proportional to inspiratory flow, due to increasing thoracic pressure as inspiratory progresses to its peak. This is easily visualized on the flow rate graph in Oscar as a flattening or declining flow rate, even as respiratory effort increases. Pressure support offsets this vacuum and prevents occlusion of soft tissue in the upper airway. The lower pressure during exhale (cycle) is not especially important to flow limitation, but without the pressure reduction, there would be no ability to have inspiratory pressure support. This lower pressure makes expiration easier, but exhale is basically a passive activity, and the muscles do not engage to cause it. The airway is under positive pressure during exhale, and expiratory obstruction is relatively rare, with some exceptions like palatal prolapse.
EPR is another name for pressure support but is set based on reduced pressure during expiration, when the real benefit is, exactly like bilevel, pressure support during the inspiratory phase. Another view is that a less efficient exhalation leads to limited inhalation or a particular inhalation flow limitation. This is particularly true where lung compliance is compromised by conditions such as COPD.
The use of EPR is best understood as a pure bilevel implementation, but Resmed avoids that because they are selling "CPAP", and their medical approval of EPR has been ensconced as a "comfort feature". As a result, it is important to establish a minimum EPAP that provides adequate airway patency when inspiration begins (trigger). Many CPAPs, and the theory of V-COM is to restore the CPAP pressure before trigger occurs. This is why Philips and other CPAPs that do not provide inspiratory pressure support fail to resolve flow limitation and the reason why this forum has very strongly advocated Resmed as a better solution...you are getting a free bilevel. The important thing is to disregard that this is a CPAP and to treat it as a bilevel in titration and use. Member "Dormeo" perhaps found the best description of EPR, "EPR reduces pressure when you exhale, but by the same token, it increases pressure when you inhale. It's the increased pressure for inhalation that helps reduce flow limitation".
References
- ↑ "Treatment of sleep-disordered breathing with positive airway pressure devices" https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4629962/

Donate to Apnea Board